.jpg)
FEMALE PELVIC ANATOMY
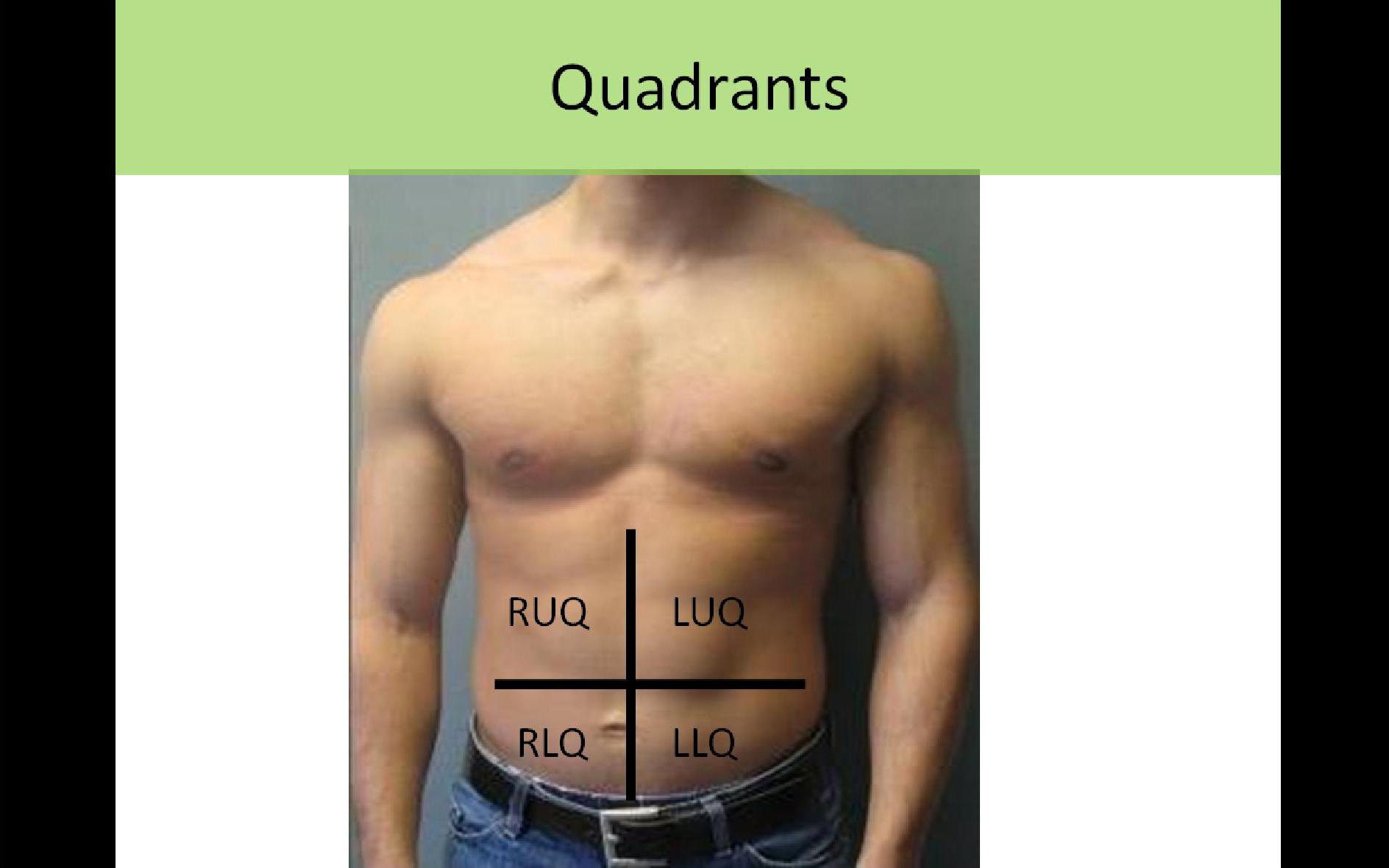
Commonly Used Quadrant Terminology:
RUQ - Right Upper Quadrant
RLQ - Right Lower Quadrant
LUQ - Left Upper Quadrant
LLQ - Left Lower Quadrant
***Abdomen divided by sagittal plane crossing through midline at umbilicus and a transverse plane crossing through the abdomen at the level of the umbilicus
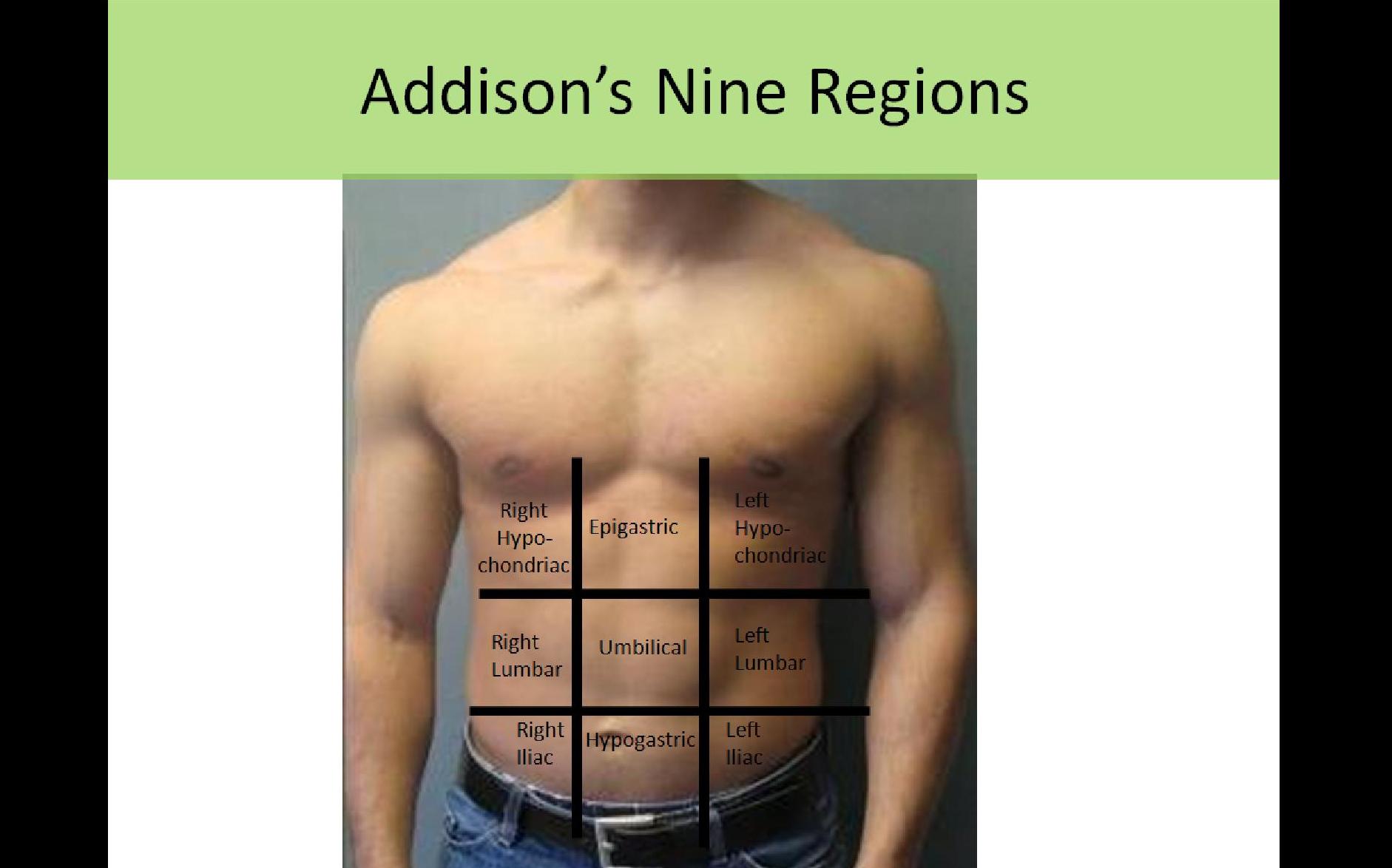
Addison's Nine Regions:
Right Hypochondrium - liver, GB, hepatic flexure of colon
Epigastric - pancreas, stomach, transverse colon
Left Hypochondrium - spleen, stomach, left kidney (upper pole)
Right Lumbar - right kidney, ascending colon
Umbilical - Transverse colon, small bowel
Left Lumbar - left kidney (mid/lower poles), descending colon
Right Iliac - ovary, seminal vesicle
Hypogastric - bladder, uterus, prostate, rectum, sigmoid
Left Iliac - ovary, seminal vesicle
ANATOMY
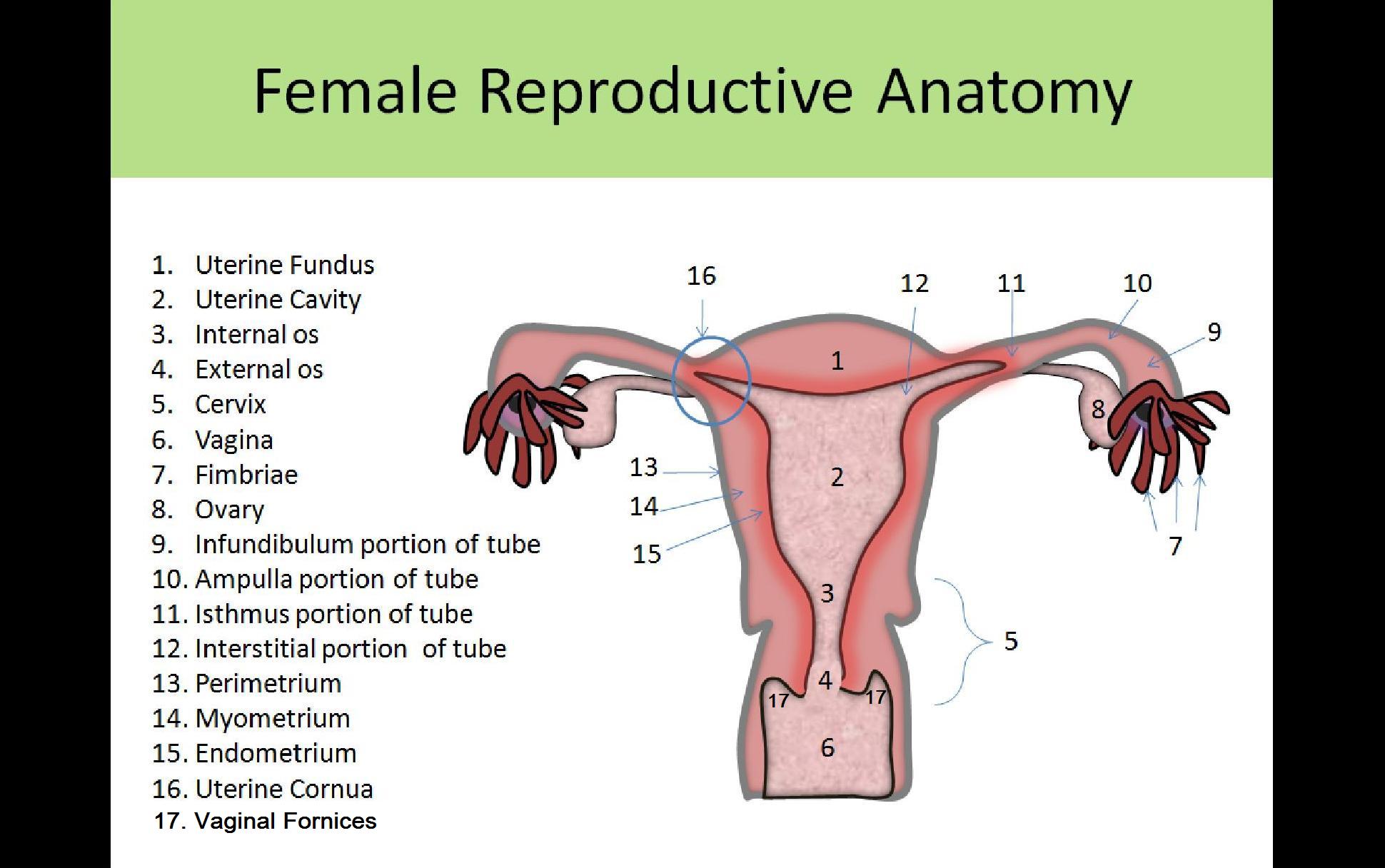
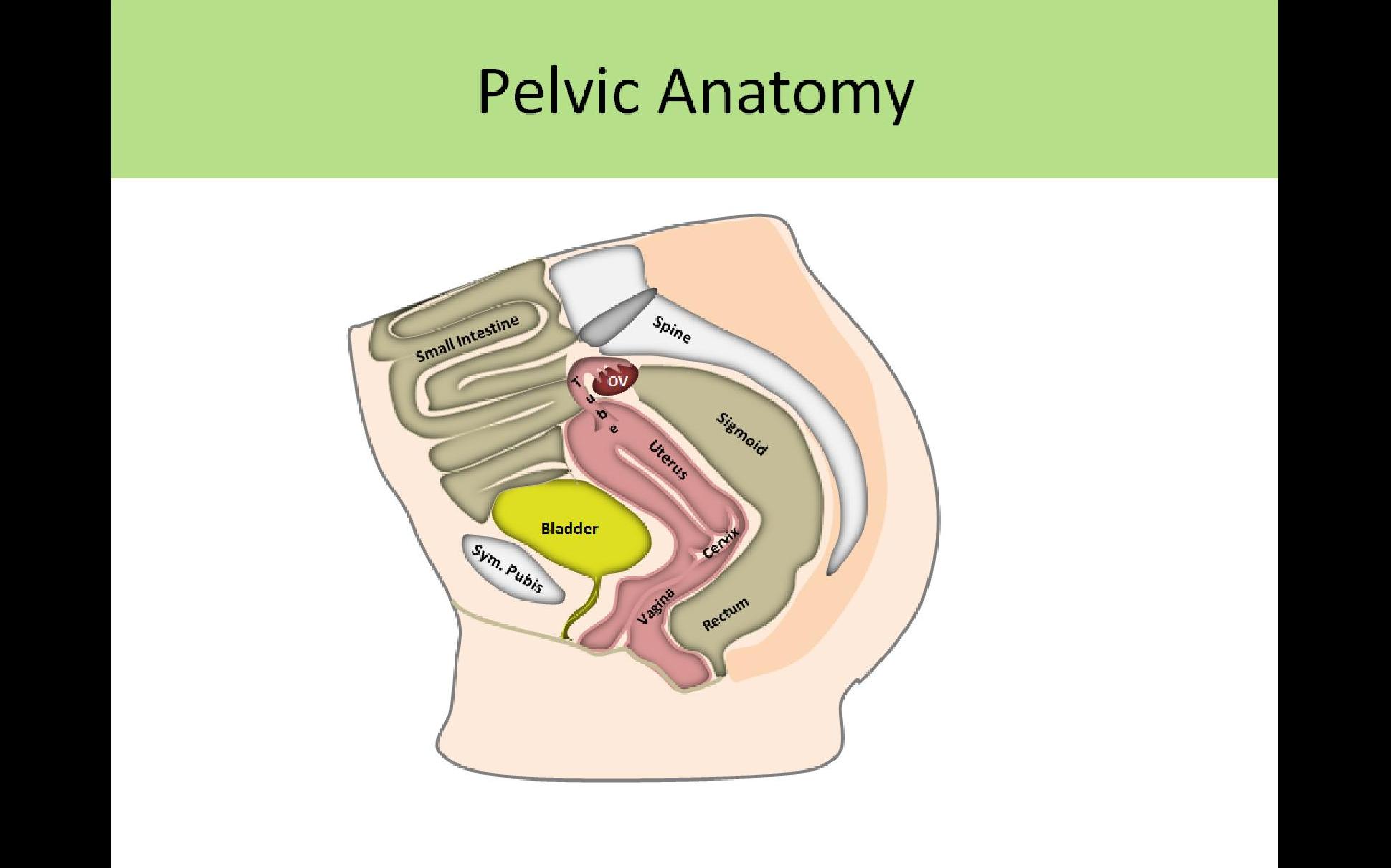
Internal Organs:
- Uterus
- Fallopian Tubes
- Ovaries
- Vagina
- Accessory Glands
- Skene's glands-paraurethral gland
- Bartholin's glands-on either side of vagina
- Mammary glands- within the breasts
External Structures:
- Mons Pubis- fatty prominence covering the symphysis pubis
- Labia Majora- outer lips covering vaginal opening
- Labia Minora- inner lips, smaller
- Clitoris- lies below the junction of the labia majora
- Linea Terminalis- imaginary line connecting superior sacrum to symphysis pubis, separates true and false pelvis
Greater/False Pelvis:
- Above the pelvic brim
- Communicates with the abdominal cavity
- Contains sigmoid colon and ileum
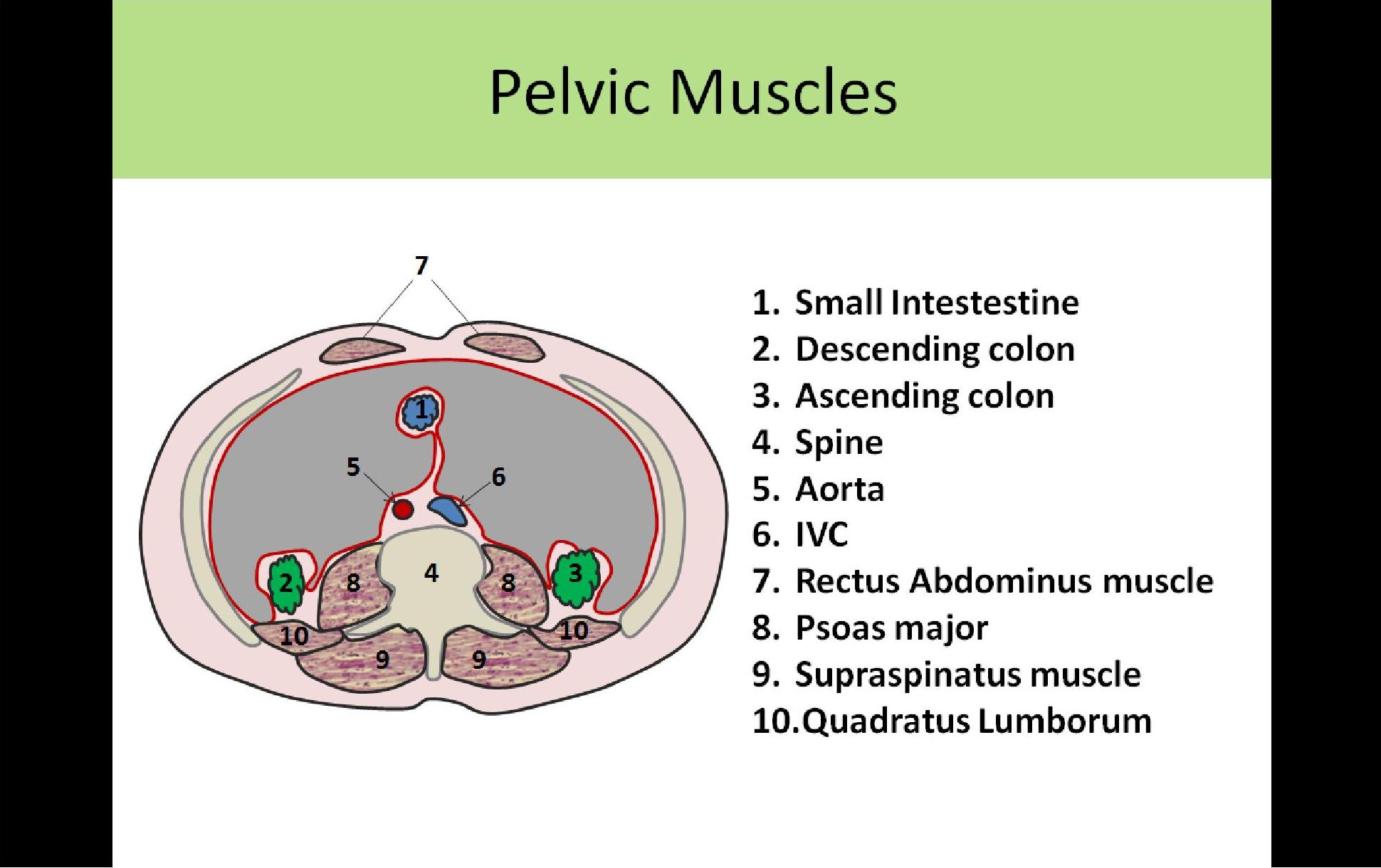
- Muscles
- Rectus Abdominis - forms anterior wall of abdominopelvic cavity, from xiphoid to symphysis pubis
- Transverse Abdominis - form the anterolateral borders of the abdominopelvic cavity
- Psoas Major - 2 muscles (left and right) originate in lumbar vertebral region and extend to the iliac crests;
- Iliopsoas - psoas muscle connects with iliacus muscle to form iliopsoas muscle
Lesser/True Pelvis:
- Below the pelvic brim
- Formed by the bony bowl of the pelvic bones
- Enclosed inferiorly by membranes and muscles
- Contains uterus, vagina, fallopian tubes, ovaries, rectum and bladder
- All muscles should be hypoechoic to the surrounding pelvic organs, some have visible striations
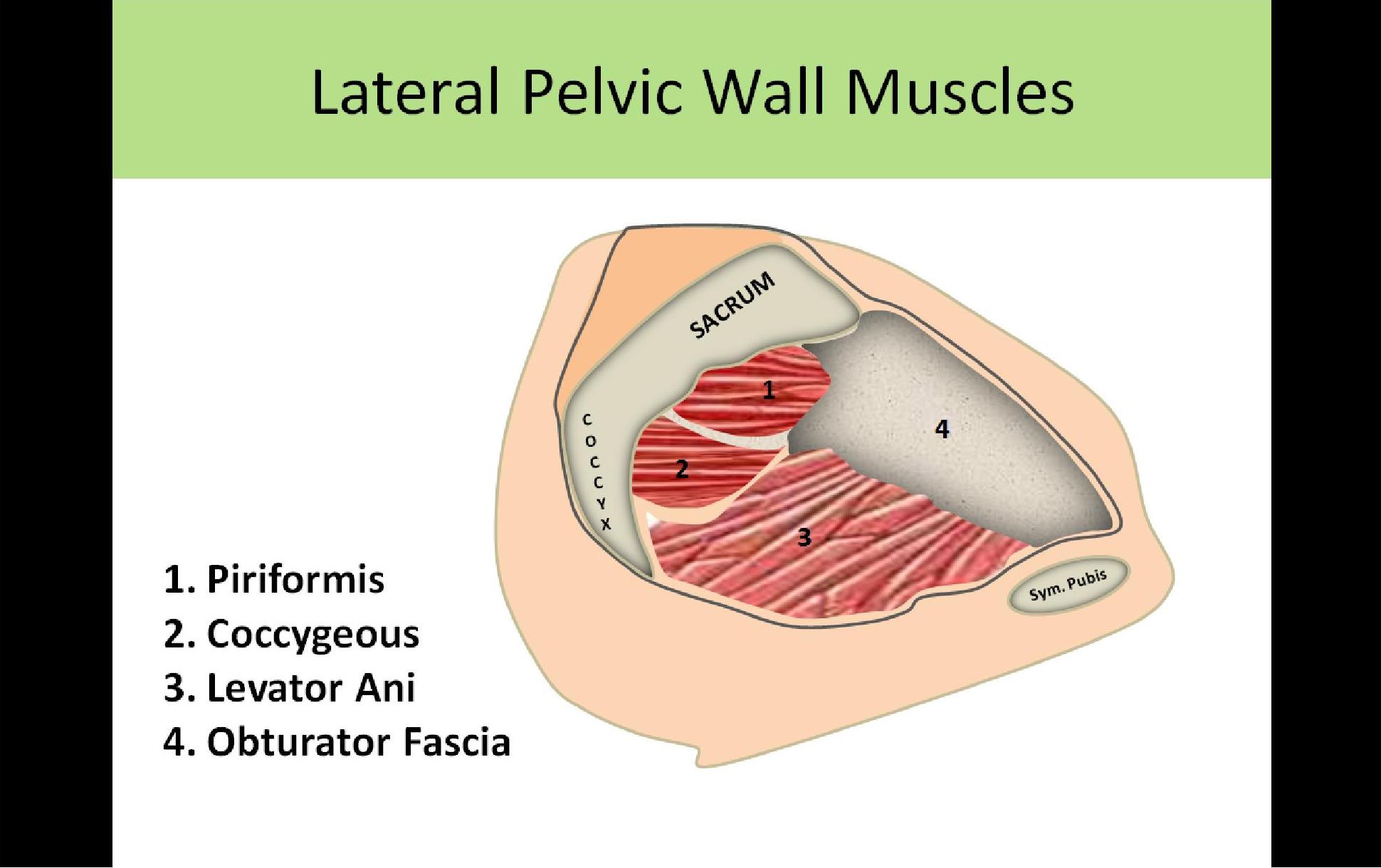
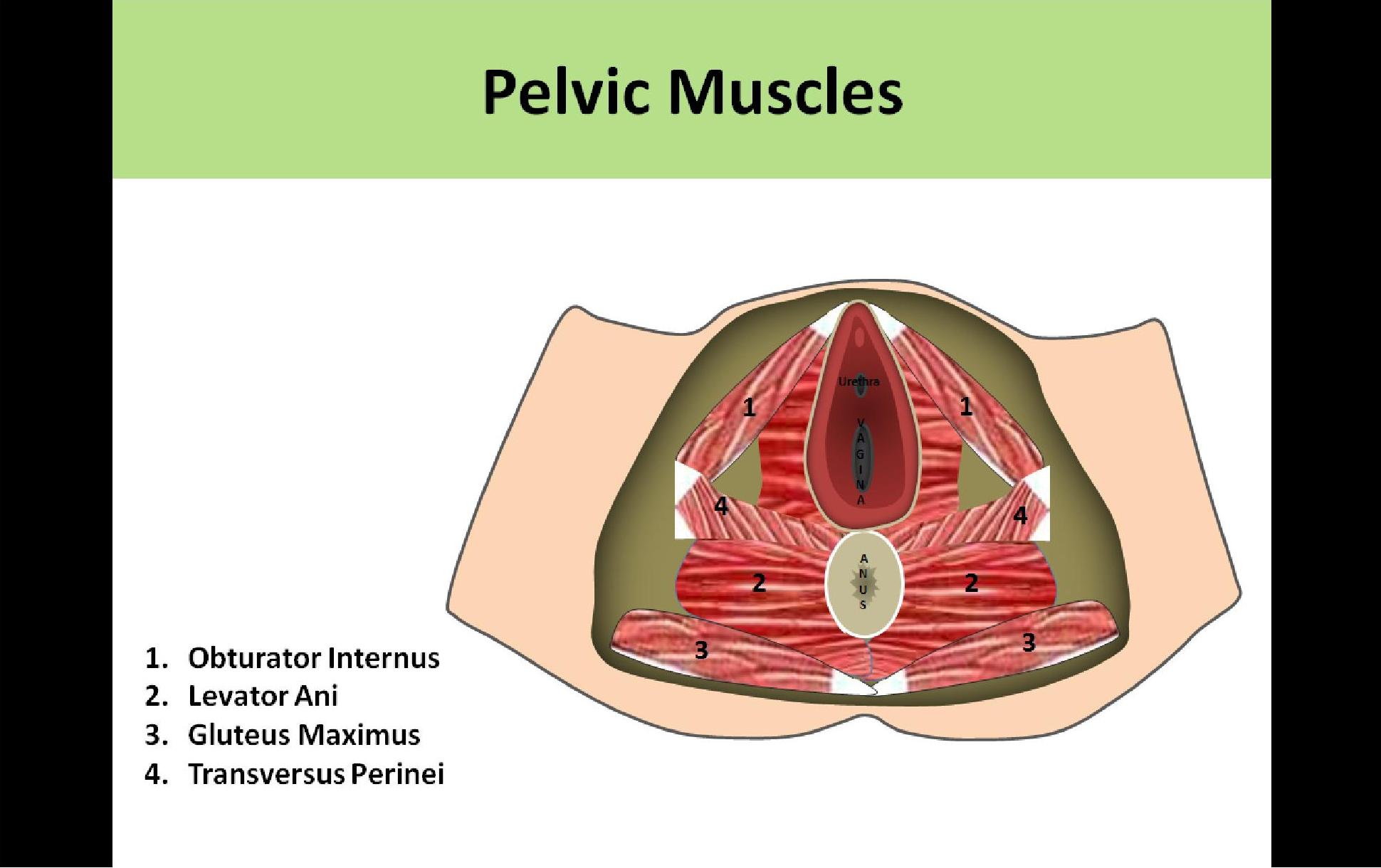
- Levator Ani
- Most inferior structure
- Pubococcygeus and Iliococcygeus muscles together are referred to as the levator ani muscles
- Connects the coccyx and the pubis bone
- Forms the floor of the pelvis
- Has 3 openings for urethra, vagina and rectum
- Can be identified on ultrasound as the flat muscle extending laterally on both sides of the vaginal cuff
- Pelvic diaphragm formed by the levator ani and coccygeus muscles
- Weakness in the levator ani muscles can lead to uterine or rectal prolapse
- Obturator Internus
- Located laterally at the acetabulum
- Triangular sheet
- Covers anterior and lateral walls of the pelvis
- Piriformis
- Superior and lateral to levator ani muscles
- Originates from sacrum and connects to the greater trochanter
- Covers posterior wall
- Most commonly mistaken for ovaries on ultrasound
- Coccygeus
- Forms the posterior portion of the pelvic wall
- Originates from the coccyx
- Psoas
- Originates in lumbar vertebral region
- Connects with the iliacus muscle to form the iliopsoas muscle
- Rectus Abdominis
- Forms the anterior abdominal wall
- Extends from the xiphoid process to the symphysis pubis
- Linea alba separates the muscles in the midline of the abdomen, extends from xiphoid to pubis
Functions of the Pelvic Skeleton:
- Provides a weight bearing bridge between spine and ribs
- Directs the pathway of the fetal head during childbirth
- Protects reproductive organs
- Innominate bones
- AKA hip bones
- Ischium
- Ilium (the ileum is in the GI tract, the ilium is a pelvic bone)
- Pubis
- Sacrum
- Coccyx
- Bones are echogenic with posterior shadowing
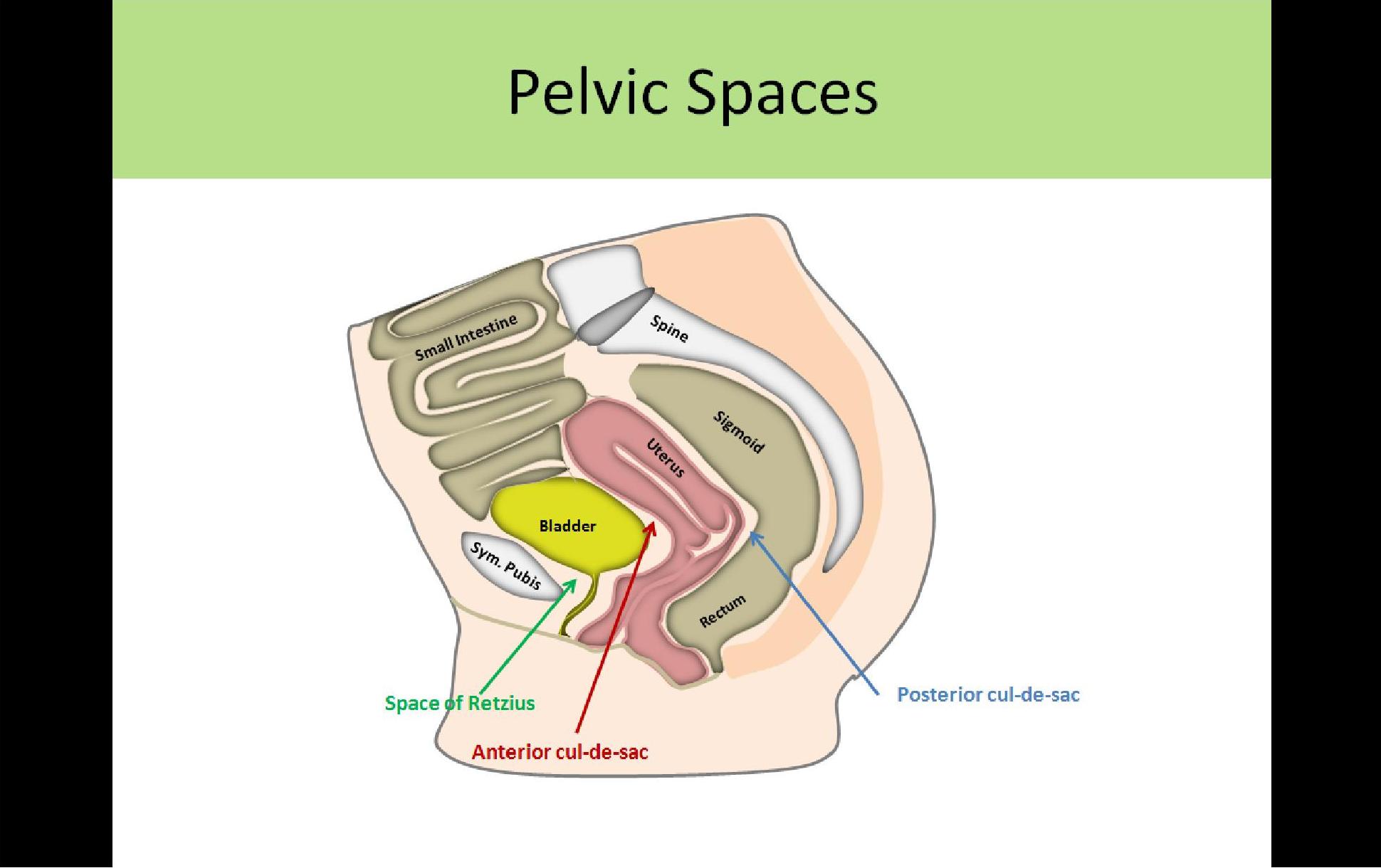
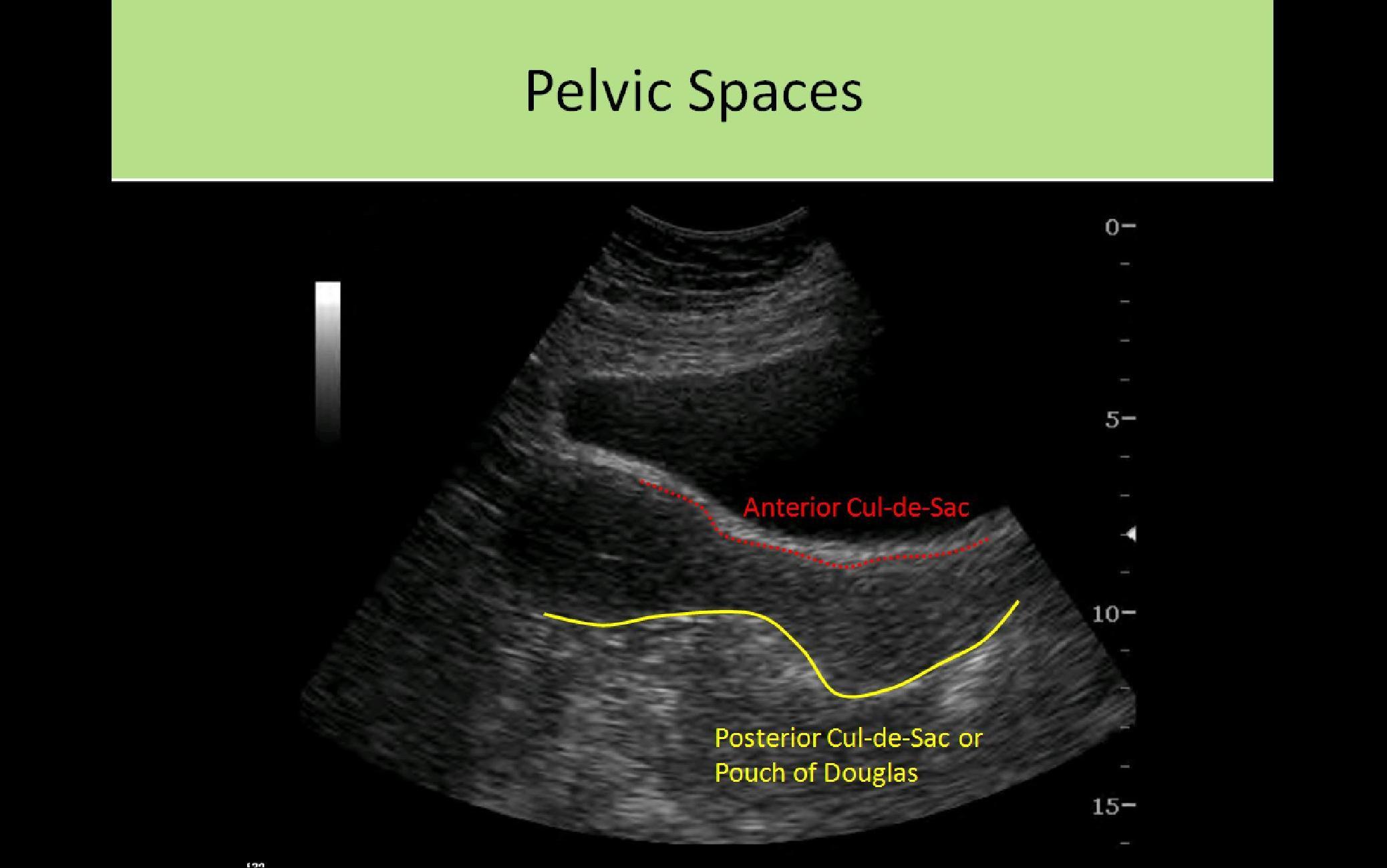
Pelvic Spaces:
- Anterior Cul-de-Sac:
- Fold in the peritoneum between anterior uterus and posterior bladder
- AKA vesicouterine pouch
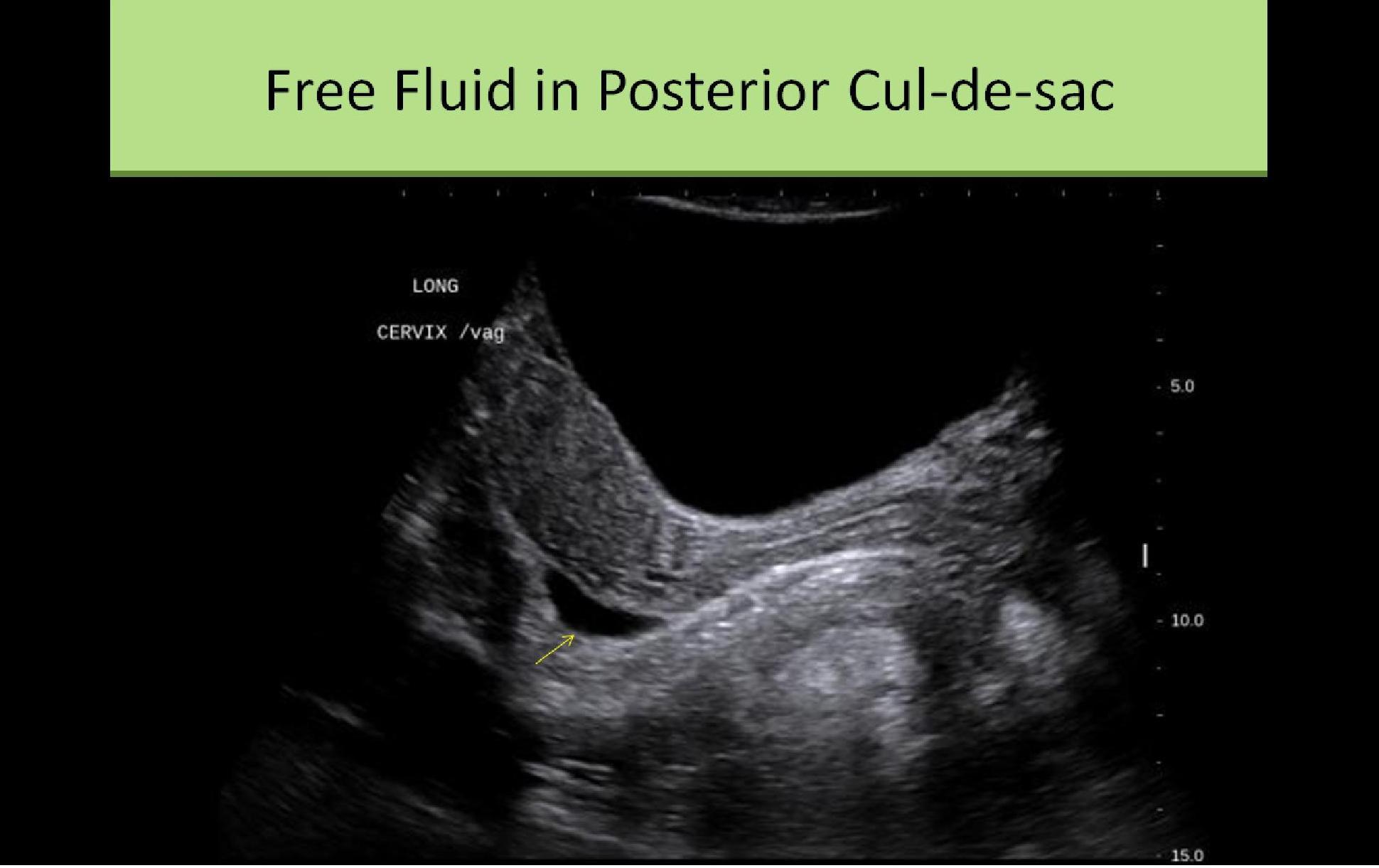
- Posterior Cul-de-Sac:
- Fold in the peritoneum between posterior uterus and anterior rectum
- AKA rectouterine pouch or pouch of Douglas
- Most dependent portion of the pelvis
- Most likely location for pooling of free fluid
- Space of Retzius:
- Anterior to bladder, posterior to symphysis pubis
- Space between the transversalis layer and outer fascia of the peritoneum
- AKA retropubic space
- Not contiguous with abdominopelvic cavity
- Very unusual for fluid collection
- Usually contains fat


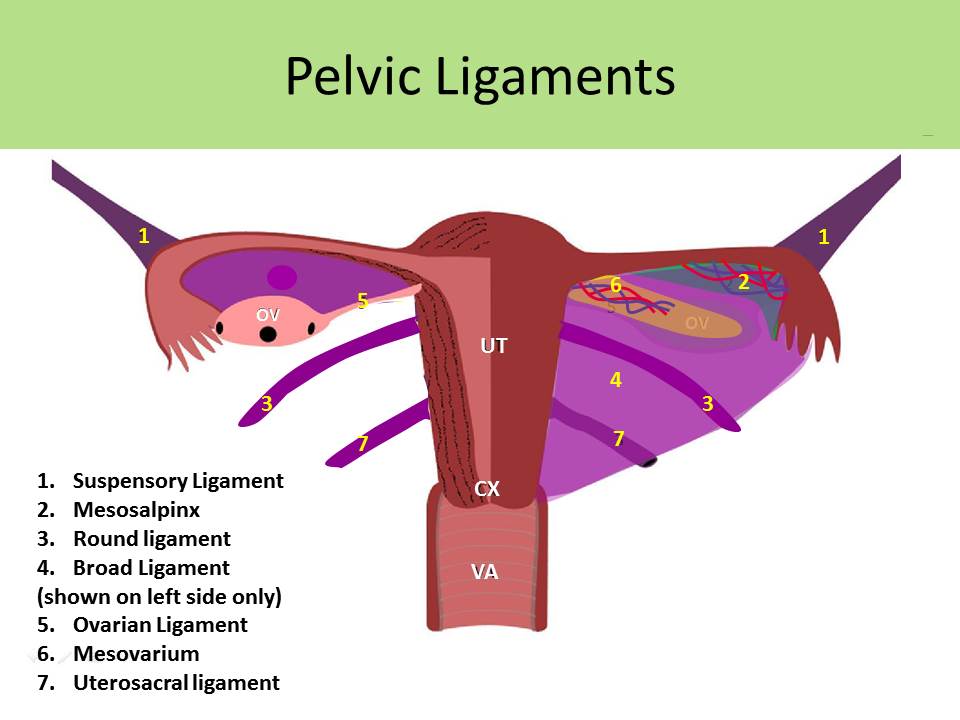
Ligaments:
Broad Ligaments:
- NOT true ligaments
- Wing like folds of the peritoneum extending from the uterine cornua to the lateral pelvic walls
- Separates pelvic cavity into anterior and posterior portions
- Covers anterior and posterior surfaces of the uterus
- Encases most of fallopian tubes and round ligament, ovarian ligament and vessels
- Loosely positions uterus in pelvic cavity and supports tubes and ovaries
- Mesovarium - portion of the peritoneum connecting anterior ovary to posterior broad ligament; contains vessels
- Mesosalpinx - free margin of the broad ligament where the fallopian tube travels; contains vessels
- Spaces within the peritoneal cavity that are posterior to the broad ligaments = Adnexa
- Fluid in the pelvis (ascites) will cause the broad ligament to become visible Sonographically
Round Ligaments:
- Fibromuscular bands extending from uterine horns to labia majora
- Maintains normal uterine fundal position and provides structural support
- Assists in birth
Cardinal Ligaments:
- AKA Transverse Cervical Ligament of Mackenrodt
- Band of fibrous tissue and muscle
- Extends from upper lateral cervix to lateral pelvic wall
- Contains the uterine and vaginal vessels
- Determines the cervix position/orientation in the pelvis with the uterosacral ligaments
Uterosacral Ligaments:
- Extend from upper cervix to lateral sacrum
- Determines the cervix position/orientation in the pelvis with the cardinal ligaments
Suspensory Ligaments:
- AKA infundibulopelvic ligament
- Folds of peritoneum that contain the ovarian vessels
- Supports fallopian tubes and ovaries within pelvis
Ovarian Ligaments:
- Lies within the folds of the broad ligament
- Supports the medial aspect of the ovary and its position relative to the uterine cornua
- Connects the medial ovary to the lateral uterine wall
Vagina Anatomy:
- Anterior to rectum, posterior to bladder and urethra
- Between the right and left levator ani muscles
- Collapsible, fibromuscular tube
- Outlet covered by hymen
- Connects to cervix at the fornix
- Walls should not exceed 1cm thickness, both measured together no greater than 2cm
- Avg cuff measurement 1.4cm
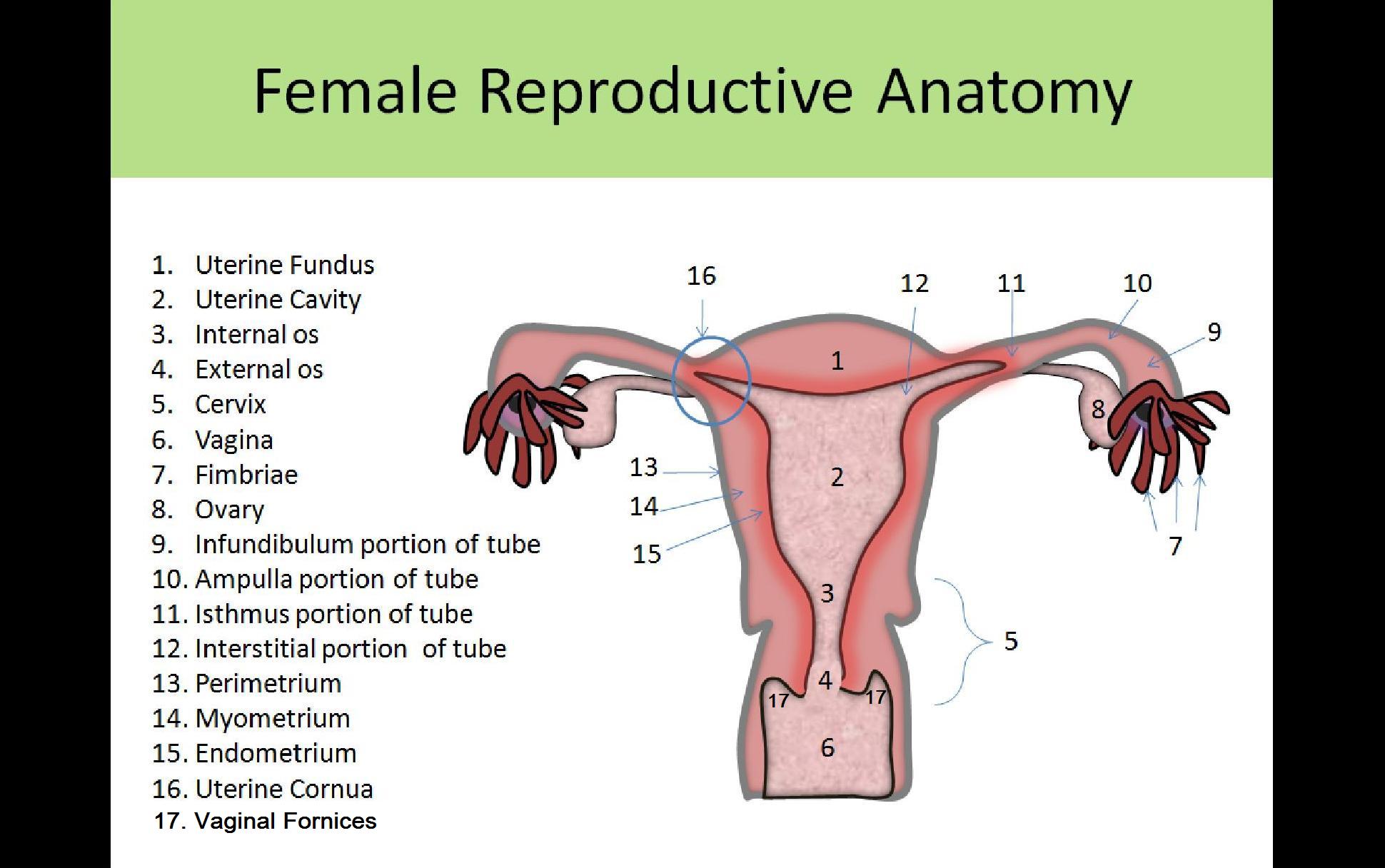
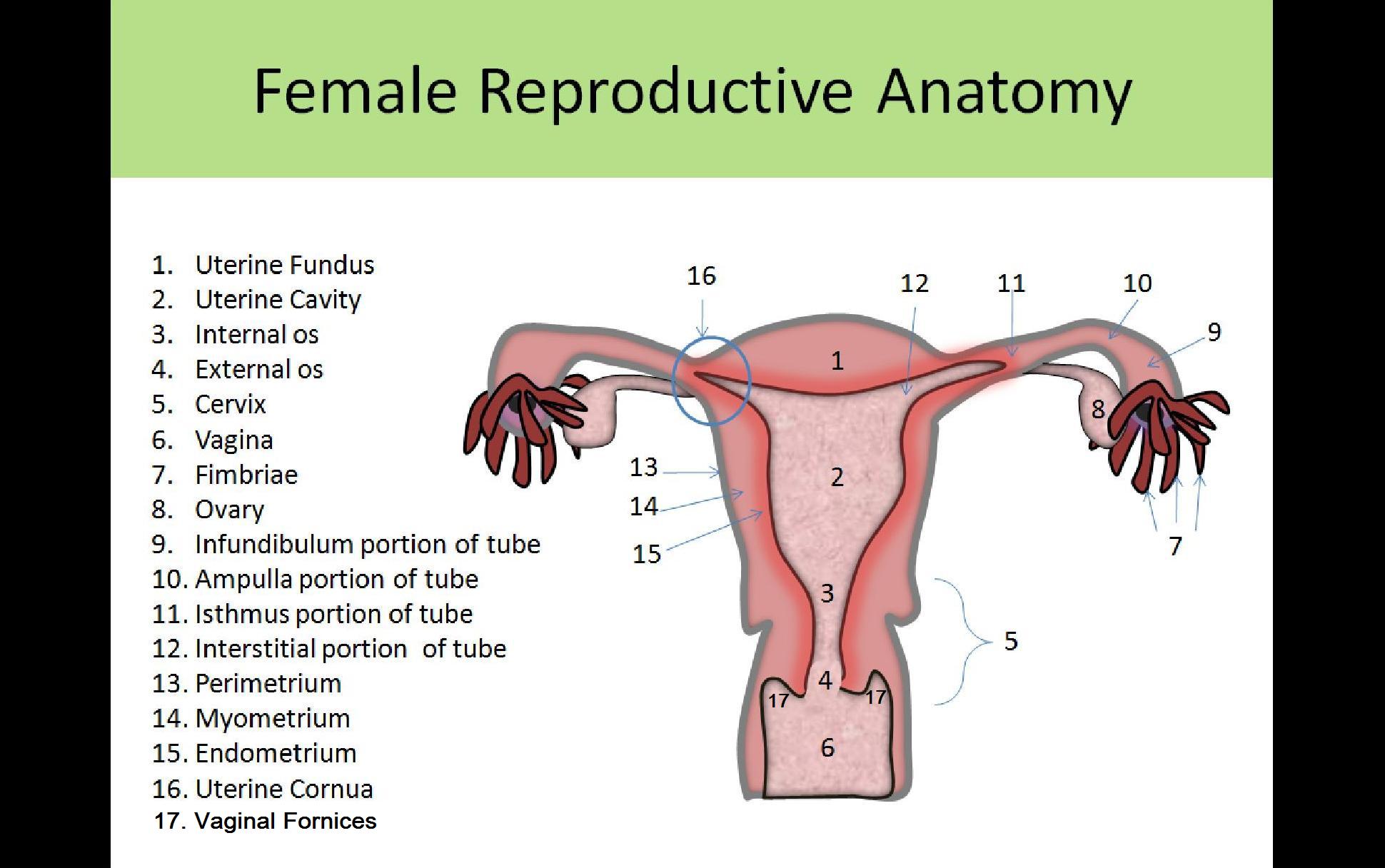
Uterine Anatomy:
- Hollow, thick-walled muscular organ
- Inner mucous layer = endometrium
- Muscle layer = myometrium
- Outer serous layer = perimetrium or serosa
- Internal os - opening from uterus into cervix
- External os - opening from cervix to vagina
- Fundus - most superior portion of the uterus above where the cornua extend into the fallopian tubes
- Body - AKA corpus; mid-section of the uterus that has great flexibility to expand with pregnancy
- Isthmus - lower portion of the corpus connected to the cervix
- Lower uterine segment - short segment between the body and the cervix in the PREGNANT patient
- Cervix connects uterine cavity with vagina
Three Wall Layers:
- Endometrium
- innermost layer
- composed of 2 layers
- superficial or functional layer - thickens and is sloughed off with menses
- deep or basal layer - not influenced by the menstrual cycle
- varies in thickness during the menstrual cycle due to proliferation and sloughing
- Myometrium
- middle layer
- thickest layer
- involved in birth
- Perimetrium
- outermost layer
- serosa
- composed of fibrous connective tissue
Location/Landmarks:
- Round, cardinal and uterosacral ligaments suspend the uterus in the pelvic cavity
- Uterus sits between two layers of the broad ligament
- Posterior to bladder
- Anterior to rectosigmoid colon
- Segmented into the fundus, corpus and cervix
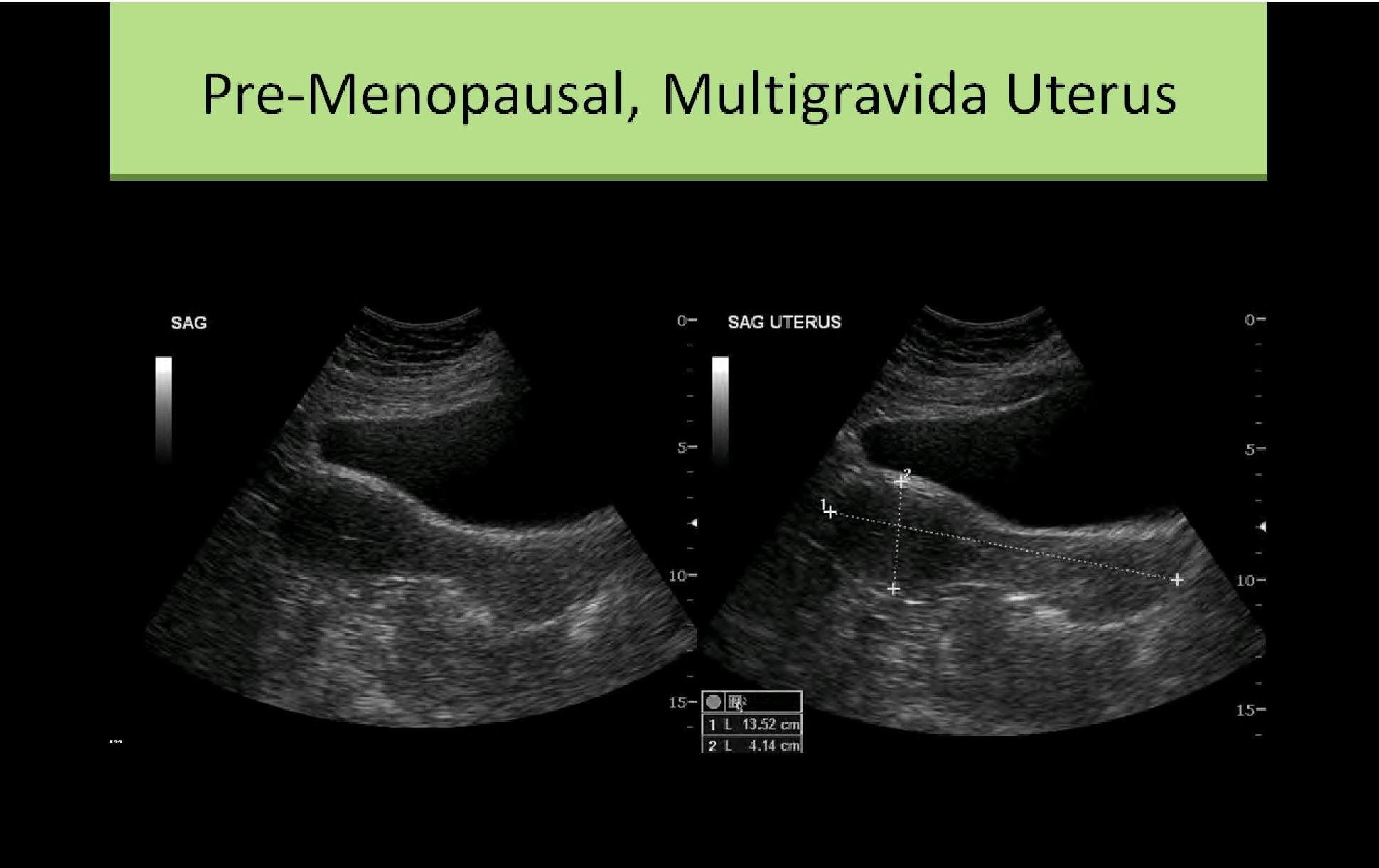
Size:
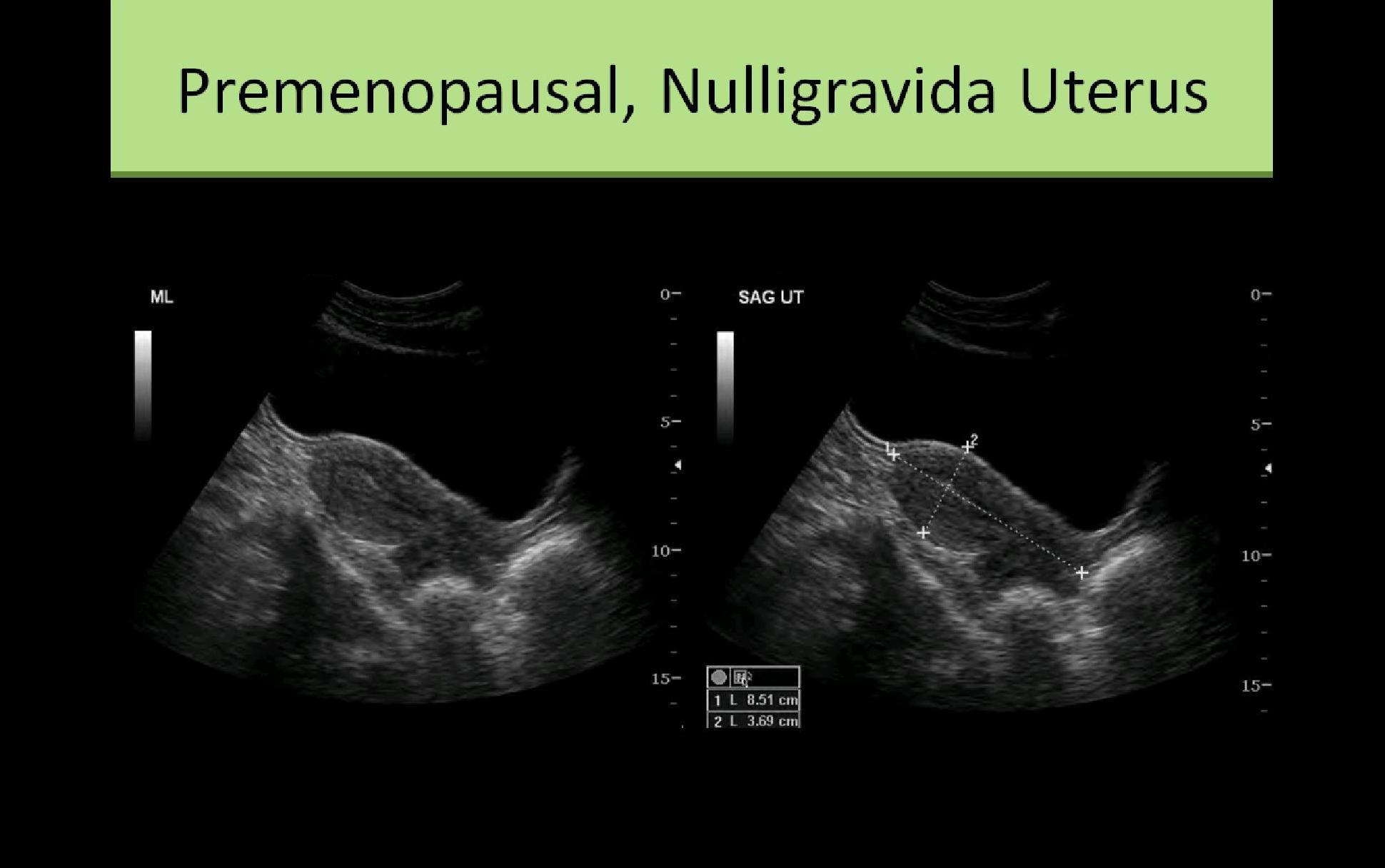
- Nulliparous
- 6 to 8.5 cm length
- 2 to 4 cm AP
- 3 to 5 cm width
- Multiparous
- 8 to 10.5 cm length
- 3 to 5 cm AP
- 4 to 6 cm width
- Measure the length in the sagittal plane, from uterine fundus to the level of the external os
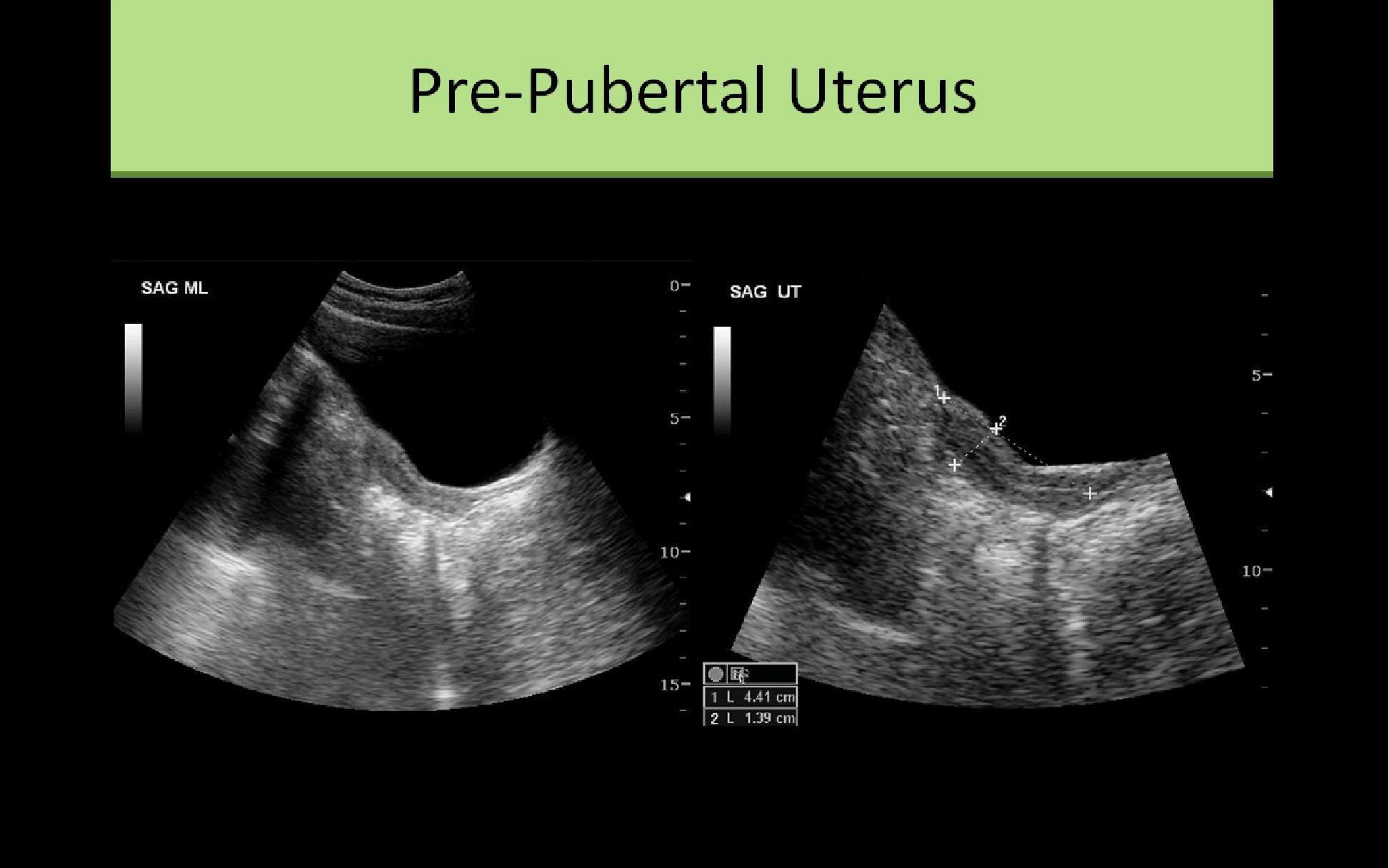
- Neonatal - Cervix more than 2X longer than the body/fundus
- Prepubertal - body half the size of the cervix
- Adult - (nulliparous) 1:1 ratio of cervix and body/fundus length
- Adult - (multiparous) body/fundus at least 2 x longer than cervix
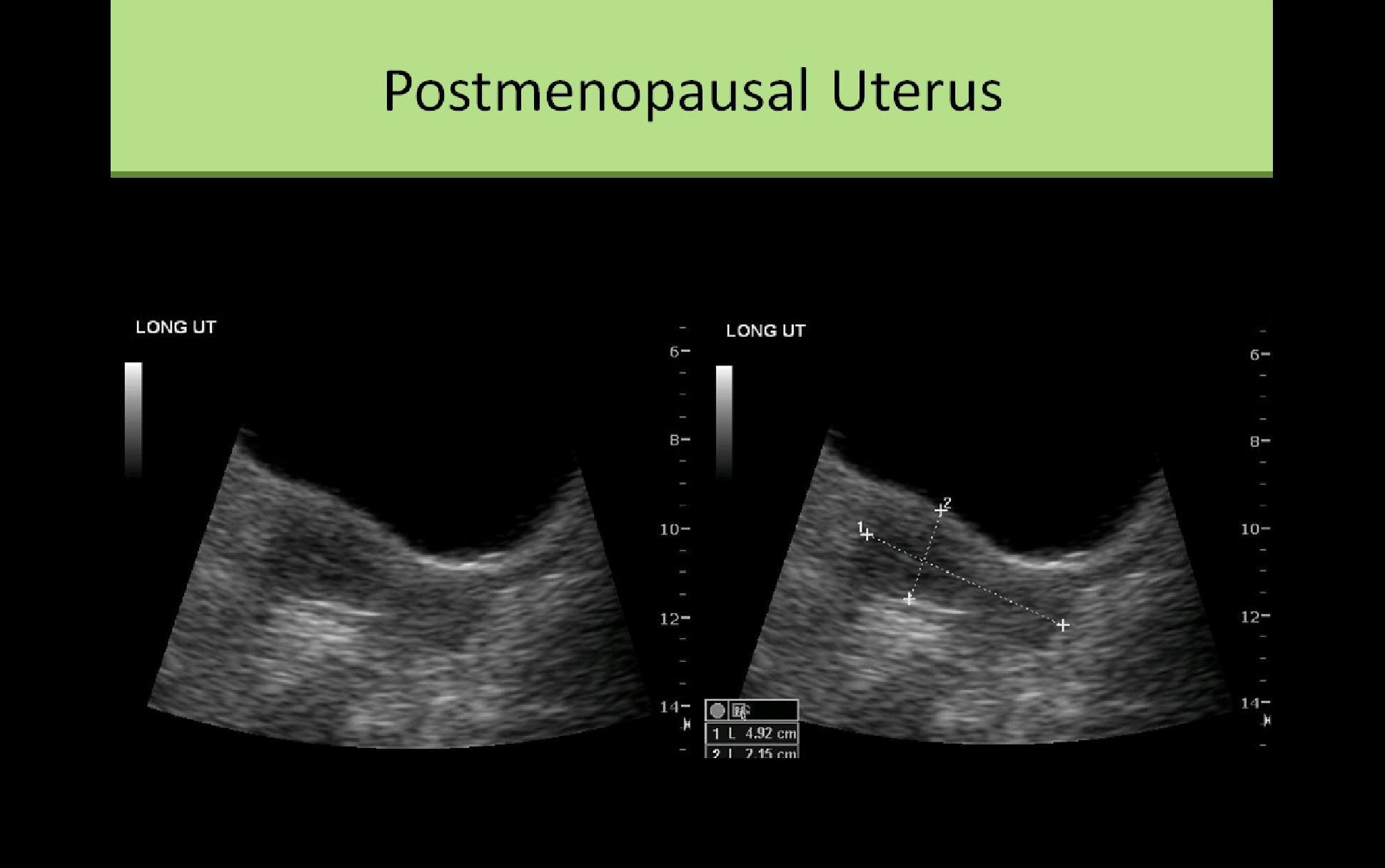
- Postmenopausal - segment ratio remains same, overall organ atrophy
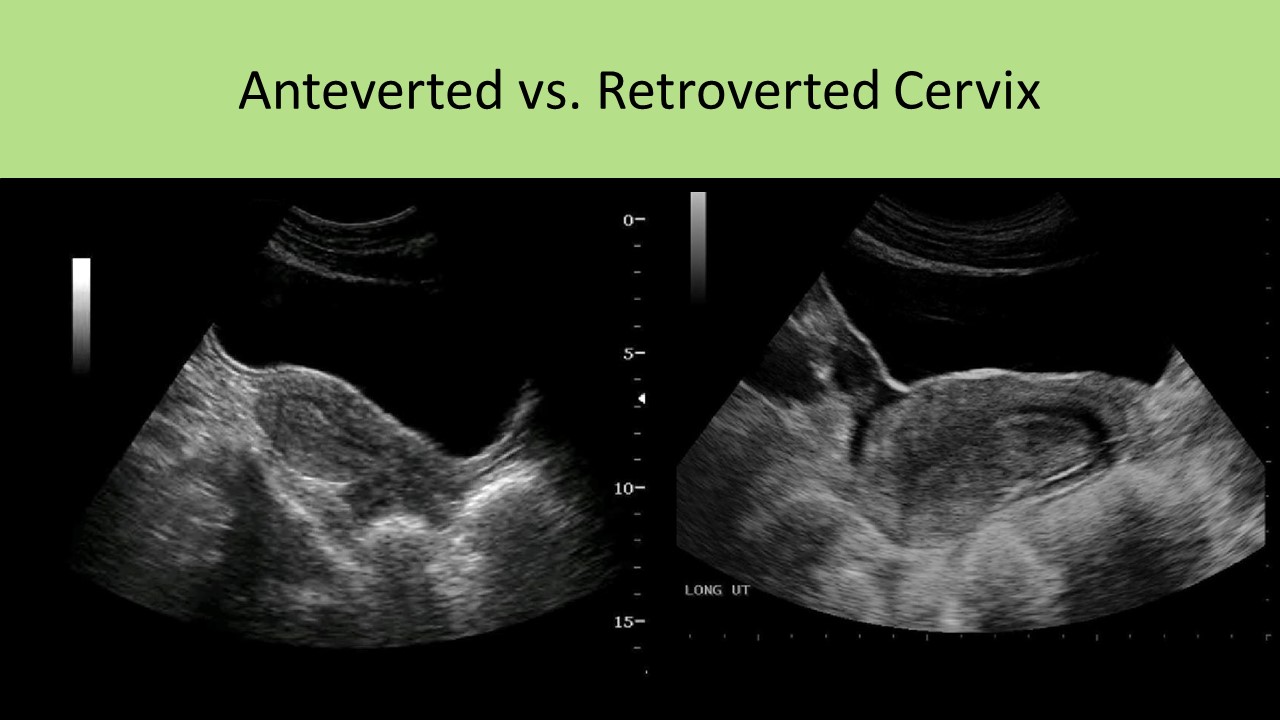
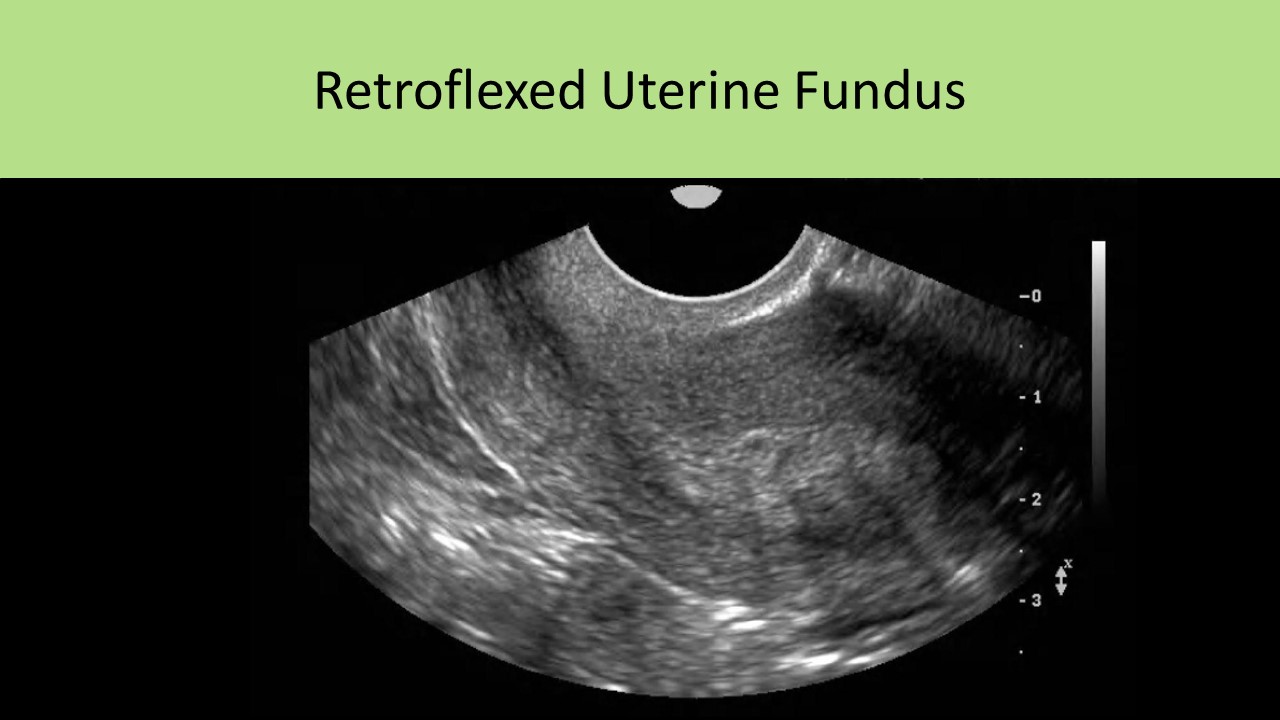
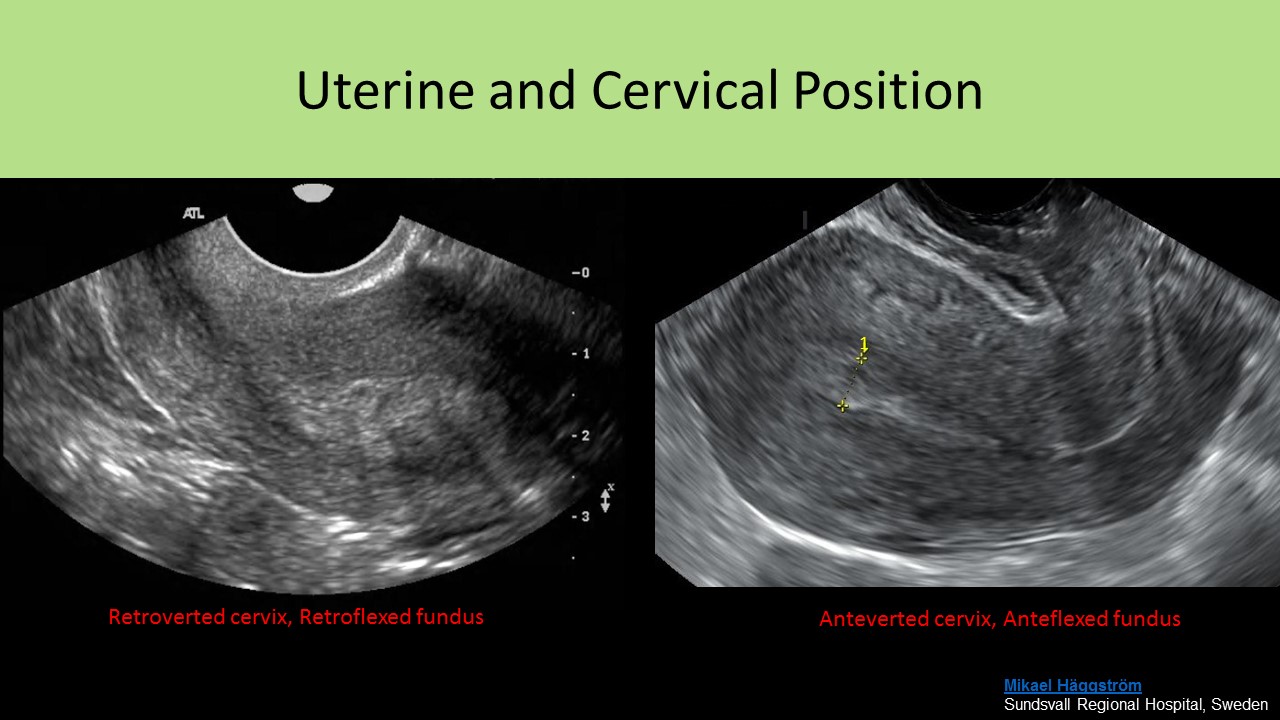
Uterine/Cervix Position:
- Anteverted - uterus forms a <90 degree angle with the cervix, cervix angles anterior from its origin at the vaginal cuff
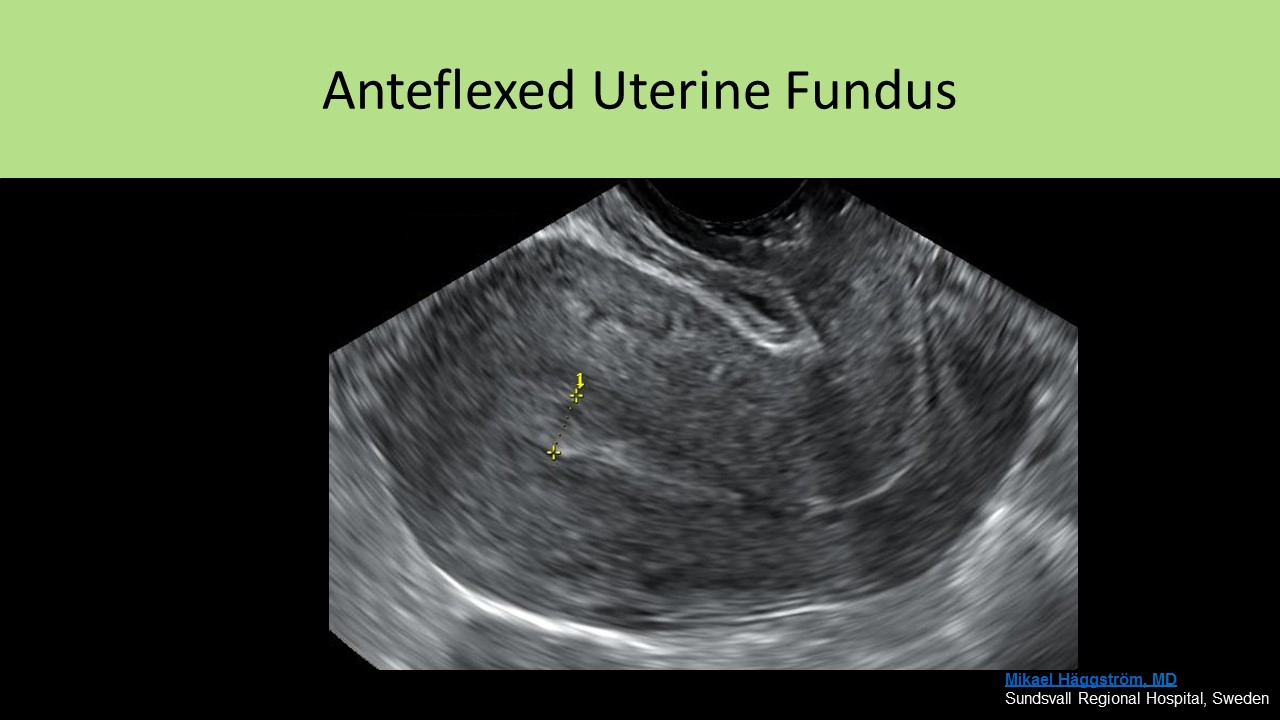
- Anteflexed - uterine body forms a sharp angle with the cervix, folds over sharply on the cervix
- Retroverted - uterine body tips posteriorly with a small angle between the corpus and the cervix, cervix angles posterior from its origin at the vaginal cuff
- Retroflexed - uterine body folds posteriorly at a very sharp angle to the cervix
- Dextroflexed - uterine body flexed to the right
- Dextroposition - entire uterus is displaced to the right
- Levoflexed - uterine body flexed to the left
- Levoposition - entire uterus is displaced to the left

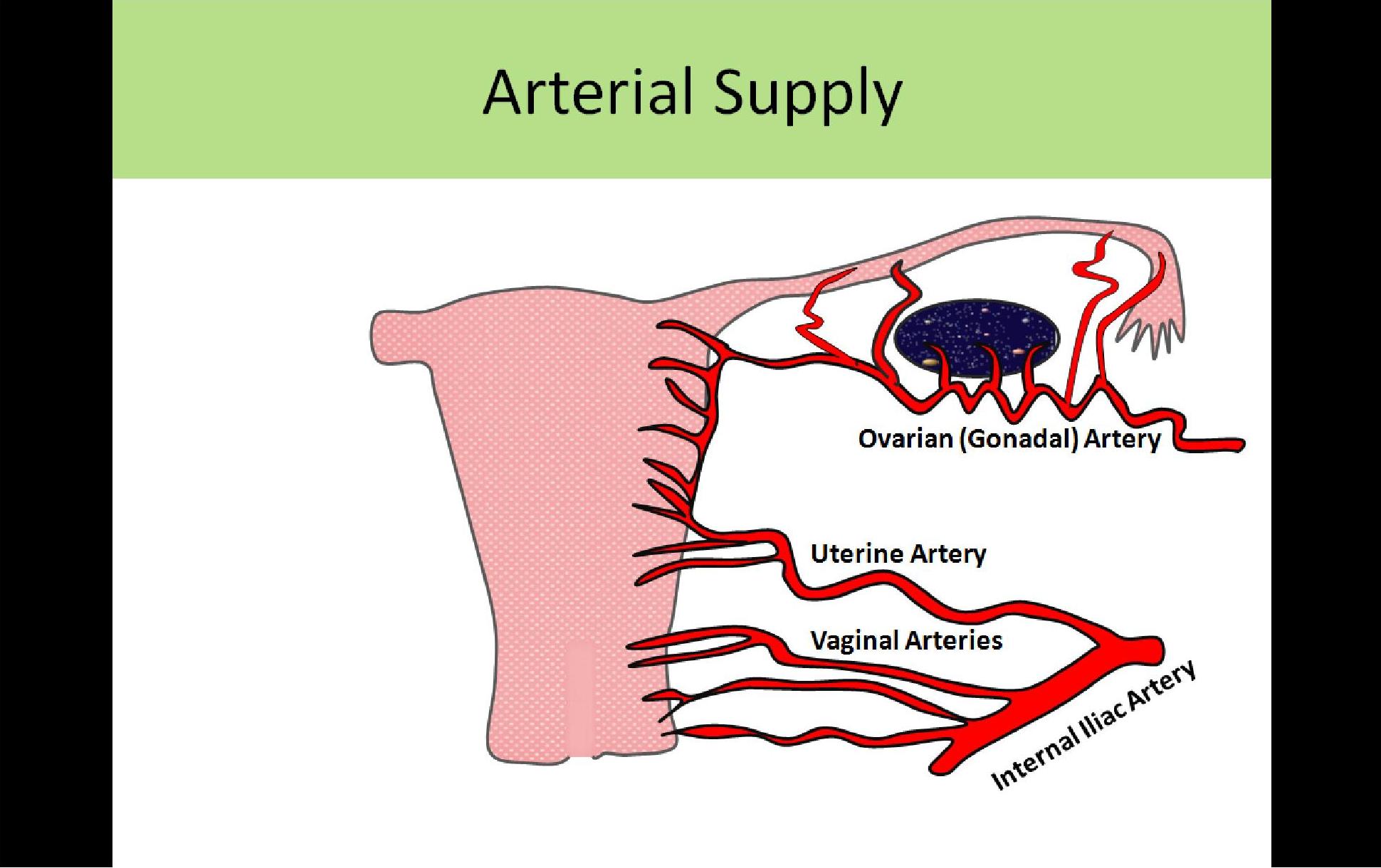
Uterine Arterial Supply:
- Uterine artery flow is of moderate velocity and high resistance
- Resistance increases with age until diastolic flow is absent or nearly absent (RI 1.0)
- In a non-pregnant patient, the internal iliac artery is smaller in caliber than the external iliac artery
- Divides into anterior and posterior segments
- Branches include the umbilical artery, inferior vesicle artery, and middle rectal artery
- The uterine artery is an anterior segment branch
- Branch of the anterior interior iliac artery
- Right and Left
- Extends to the cervix to then course superiorly along the outside of the uterus
- The vaginal artery branches from the uterine artery and supplies vagina with blood
- Small branches merge with branches of the ovarian artery near the uterine cornua
- Blood is supplied to the ovaries and tubes by the uterine artery and ovarian artery
- Gives rise to many small arcuate arteries
- Encircle the periphery of the uterus
- Course parallel to the long axis of the uterus
- Gives rise to smaller branches called radial arteries that penetrate the serosa and myometrium
- The radial arteries penetrate the myometrium and branch into the spiral and straight arteries
- Straight arteries supply the basal layer of the endometrium
- Spiral arteries supply the functional layer of the endometrium and are stimulated by the menstrual cycle
Uterine Venous Drainage:
- Uterine veins empty into the internal iliac veins
- Internal iliac veins are posterior and medial to the internal iliac arteries
- Iliac vessels are located lateral and posterior to the ovaries
- In a non-pregnant patient, the internal iliac vein is smaller in caliber than the external iliac vein
- Merges with the external iliac vein to form the common iliac vein
- Drains pelvic organs