
.jpg)
Extremity Venous Anatomy and Sonographic Evaluation
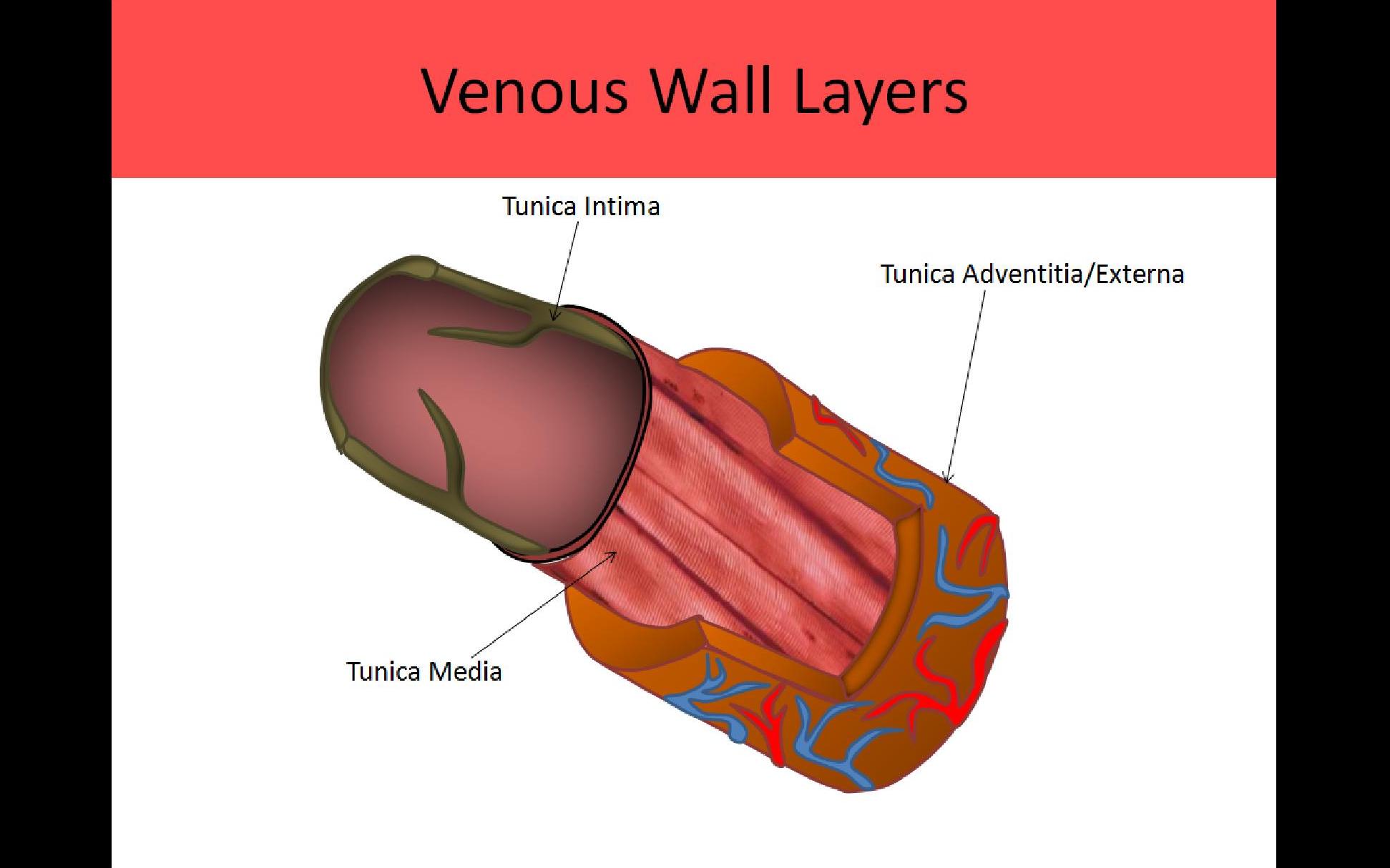
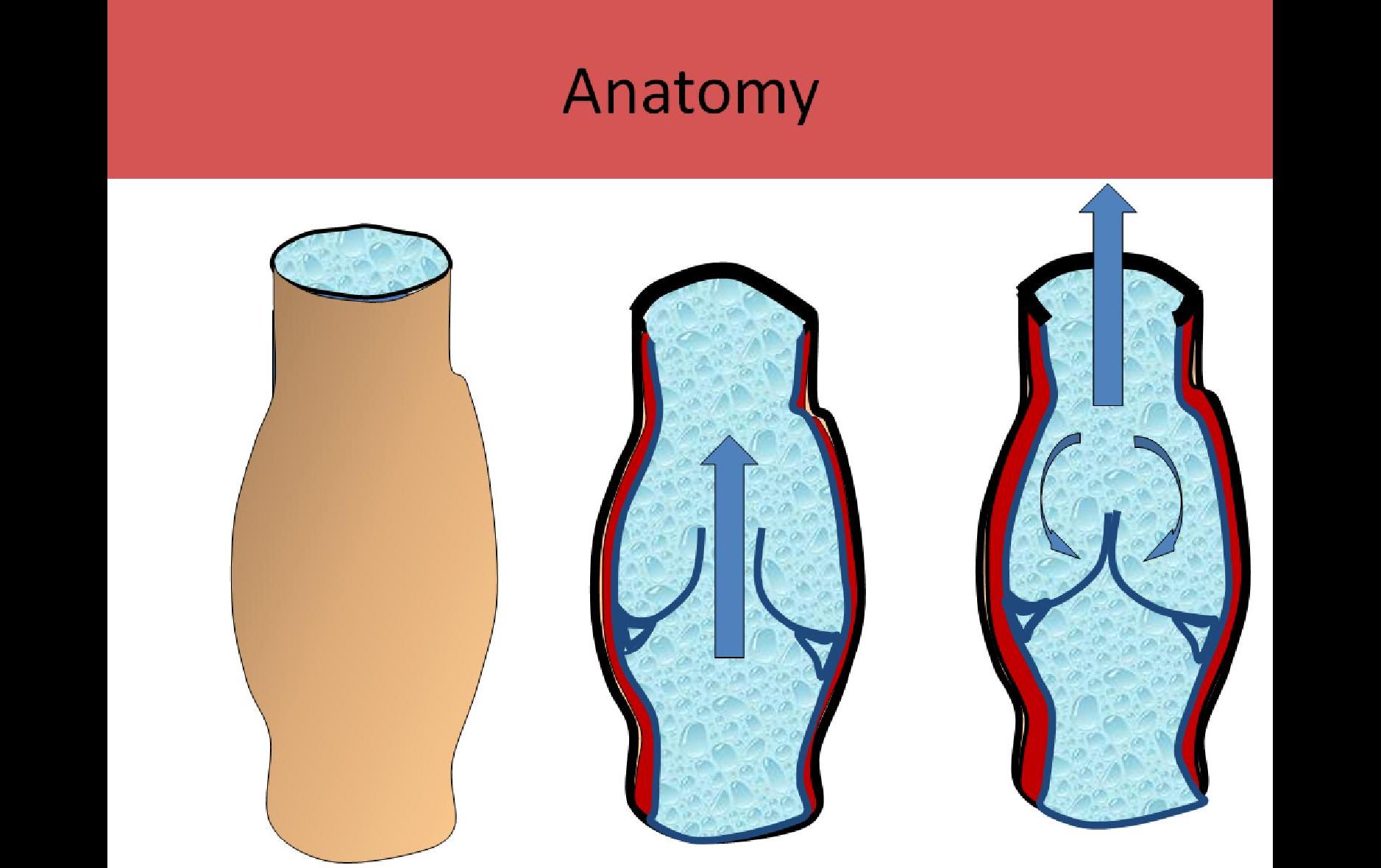
VENOUS ANATOMY:
- Thin walled, collapsible
- Still allows for some dilatation and constriction
- Media layer thinner than artery
- Walls of the upper extremity veins contain much less muscle than walls of the veins in the lower extremity and especially the feet; this is due to hydrostatic pressure
- Progressive increase in size as they get closer to heart
- Most contain valves
- Veins originate distally as venules in the extremity(hands/feet) and travel to right atrium
- Capillary beds are composed of intima only and connect to venules
- Venules are composed of intima and adventitia layers only (no media layer)
- Pressure in the venules normally does not exceed 20mmHg
- 80% of the blood in the body is found in the venous system
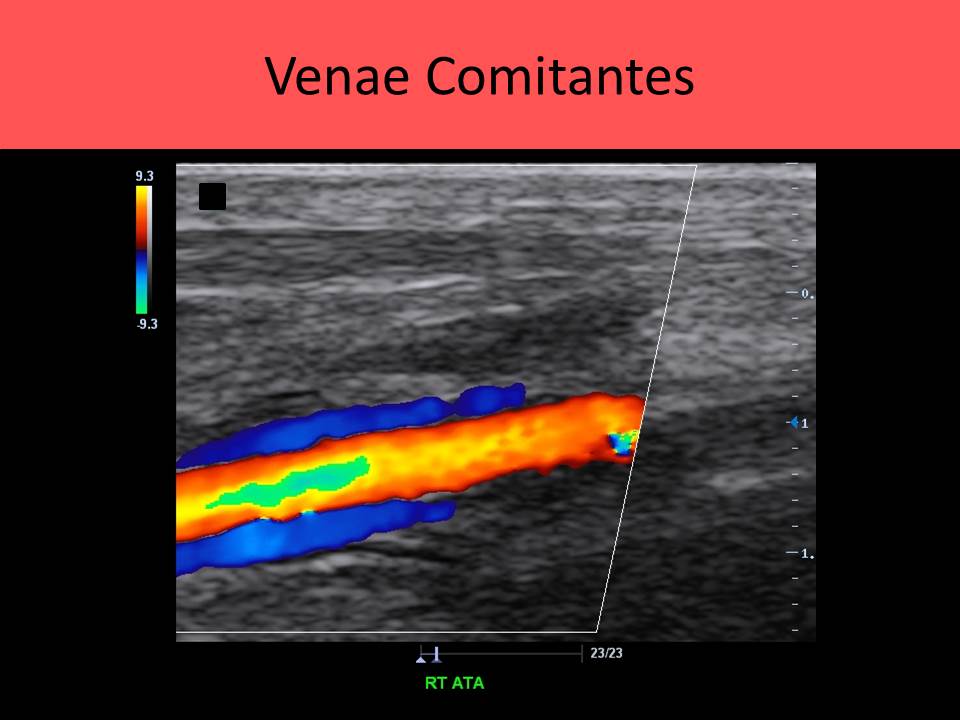
- Concomitant veins - refers to a vein that is usually paired, with a vein lying on either side of a single artery
- Radial, ulnar, PTV, ATV, peroneal and gastrocnemius veins are example of concomitant veins
***Remember proximal used to be defined as closest to the point of origin*** BUT current vascular nomenclature refers to proximal as being closest to the heart EX: The "proximal" SFV is in the upper thigh and closer to the heart than the "distal" SFV in the lower thigh
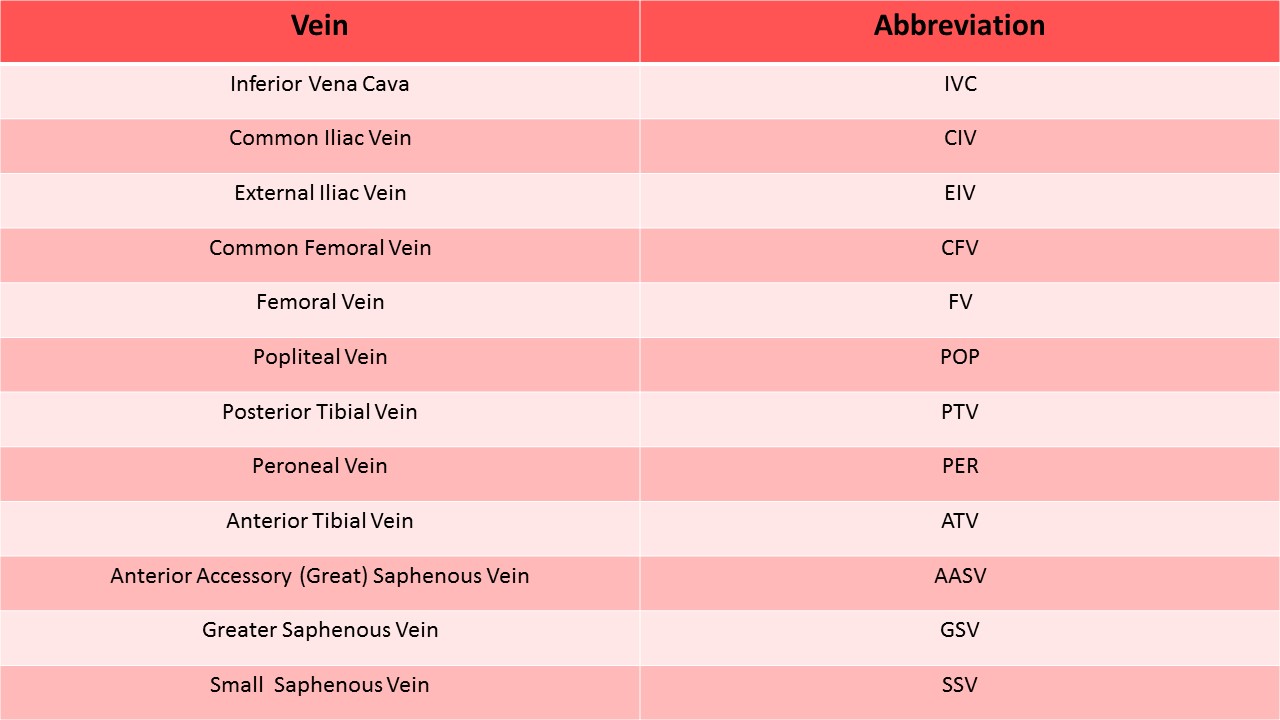
Central Veins:
- Inferior Vena Cava IVC - confluence of iliac veins
- Hepatic veins
- Superior Vena Cava SVC - confluence of innominate veins
- Portal vein-confluence of SMV and splenic vein
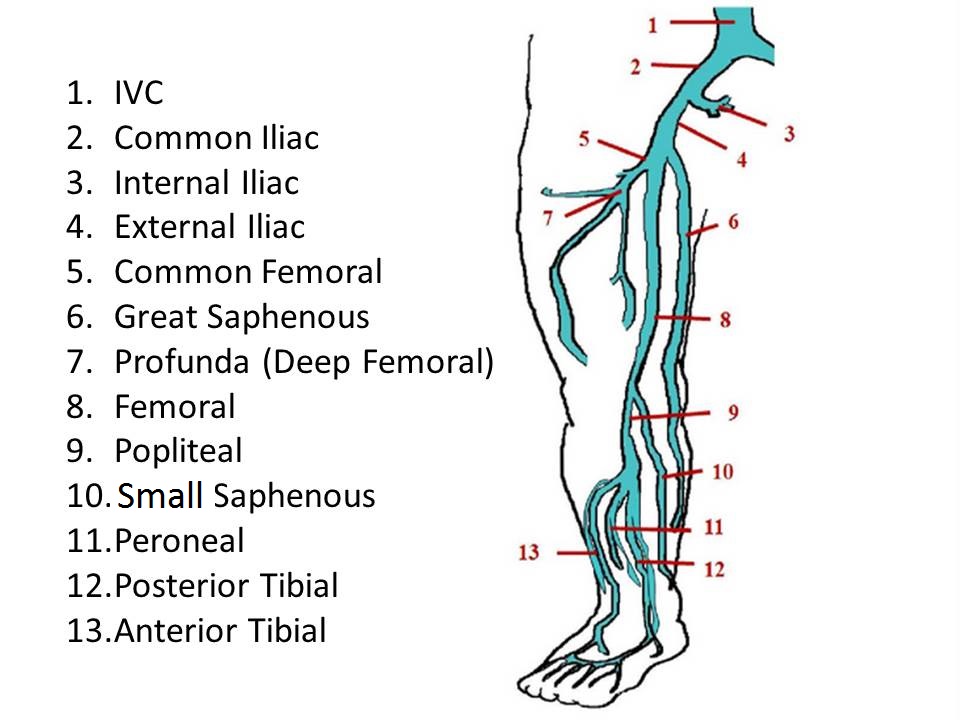
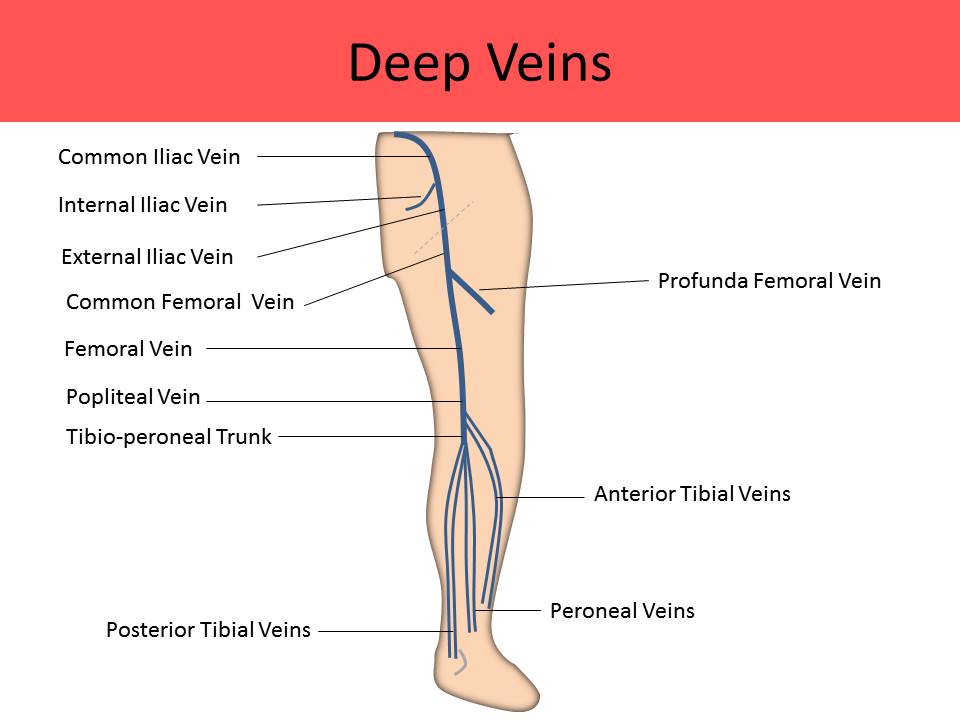
Lower Extremity Deep Veins:
Deep digital veins > metatarsal veins > Deep venous arches > PTVs and peroneal veins > tibioperoneal trunk > ATVs > popliteal vein > superficial femoral vein > common femoral vein > external iliac vein
- Veins in the lower extremity originate at the confluence of the venules of the deep digital veins
- Metatarsal veins drain the blood from the foot and merge into the deep venous arches
- Deep venous arches empty their blood into tibial veins
- Calf and forearm veins are referred to as venae comitantes because 2 veins of the same name follow the same course as a single artery of the same name
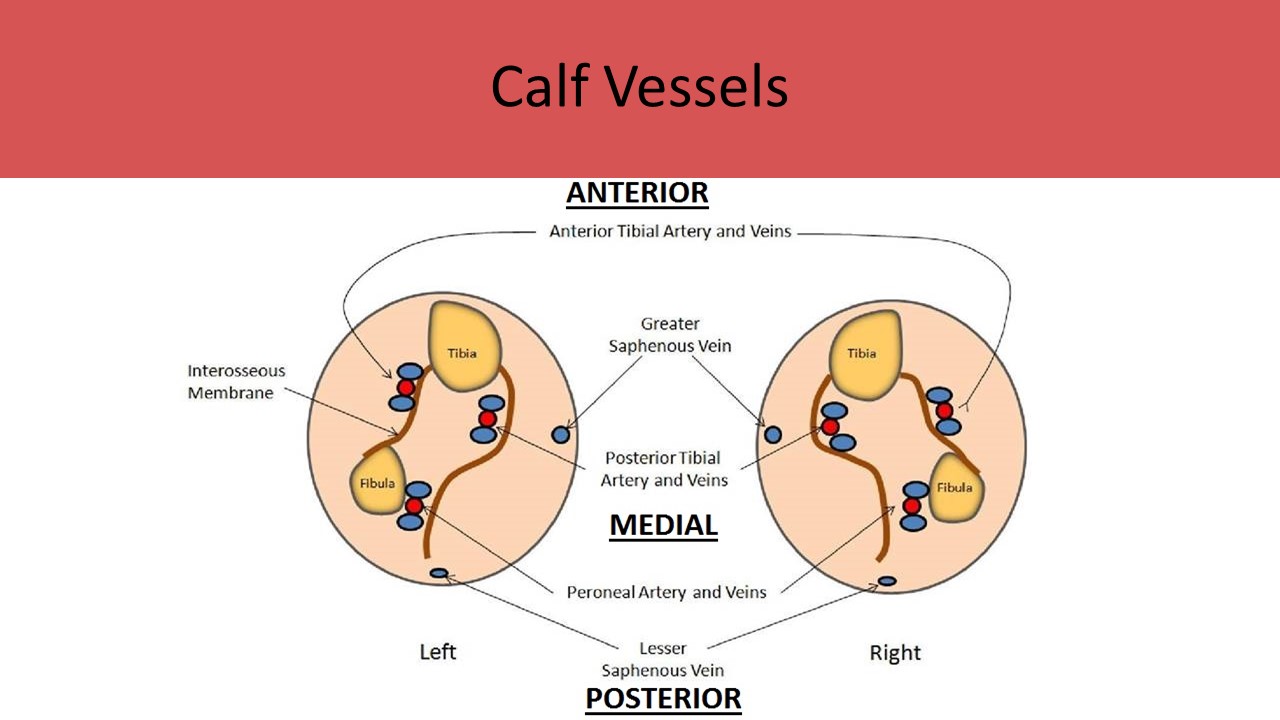
- Drain blood from the anterior calf
- 2 veins originate at the plantar arches
- Course cephalad anterolateral to the tibial bone and the interosseous membrane to reach the tibioperoneal trunk
- Travels between the tibial head and fibula head to join the popliteal vein
- Best scan approach is anterior calf with slightly lateral probe position
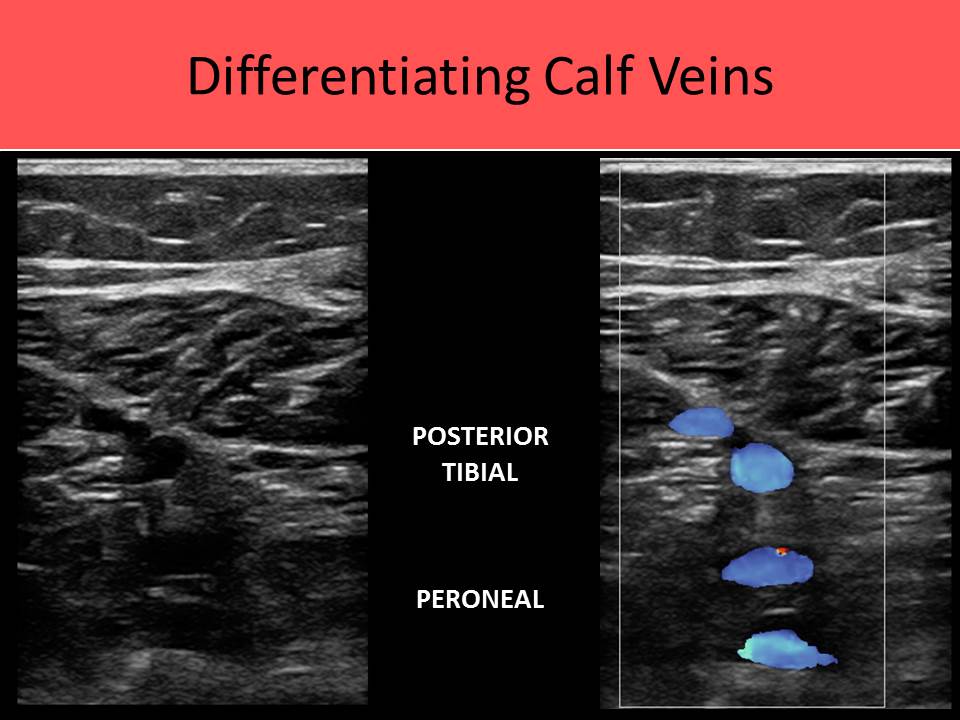
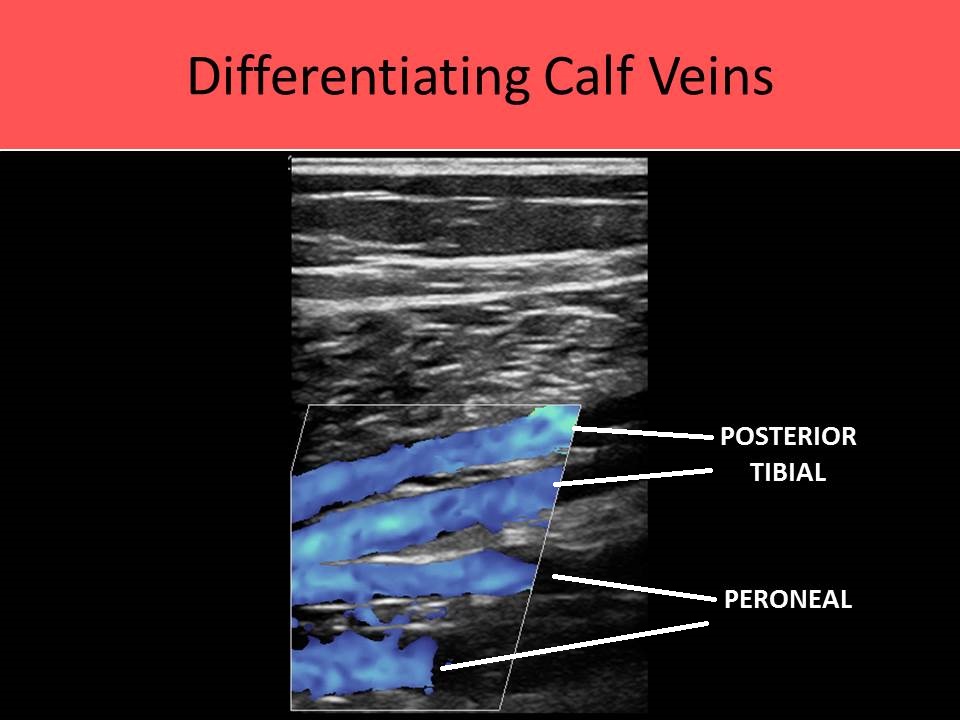
- Drain blood from the posterior calf
- 2 veins originate at the confluence of the plantar arches
- At the ankle the PTVs course posterior to the medial malleolus and anterior to the Achilles' tendon then course cephalad through the calf posterior to the tibial bone
- Best scan approach is to place probe on the medial calf, angling through to the lateral side; PTVs most anterior on image and peroneals visible beneath them
- Drain blood from the lateral calf
- In the lower calf/ankle 2 veins course lateral to the PTVs and medial to the fibula,
- Continue in a cephalad course up the midline of the posterior calf, posterior to the fibula
- 2 peroneal veins and 2 posterior tibial veins merge to form a single tibio-peroneal trunk in the upper calf
- Best scan approach is to place probe on the medial calf, angling through to the lateral side; PTVs most anterior on image and peroneals visible beneath them
- Tibioperoneal trunk merges with the two anterior tibial veins to form the popliteal vein in the popliteal fossa
- Courses posterior to the popliteal artery
- Becomes the femoral vein at adductor hiatus in the distal thigh
- Best scan approach is to place probe on the posterior popliteal fossa; popliteal vein demonstrated ANTERIOR to the popliteal artery on the image due to the scan approach
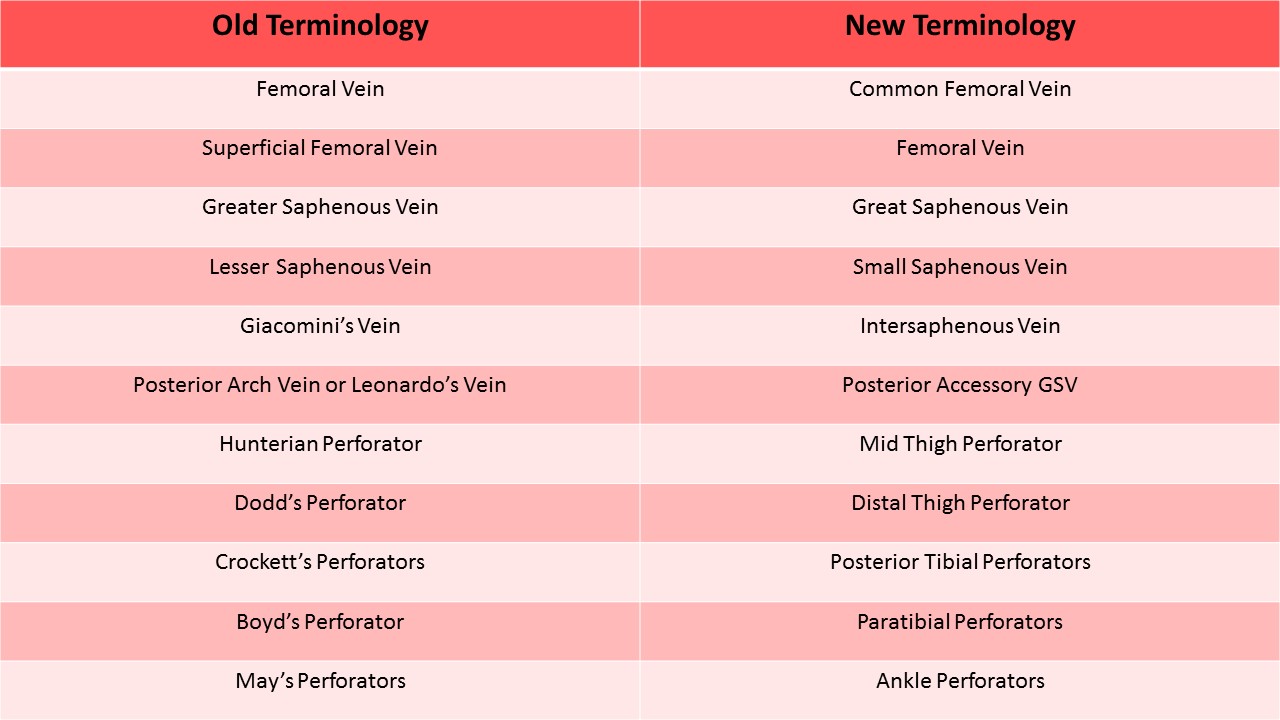
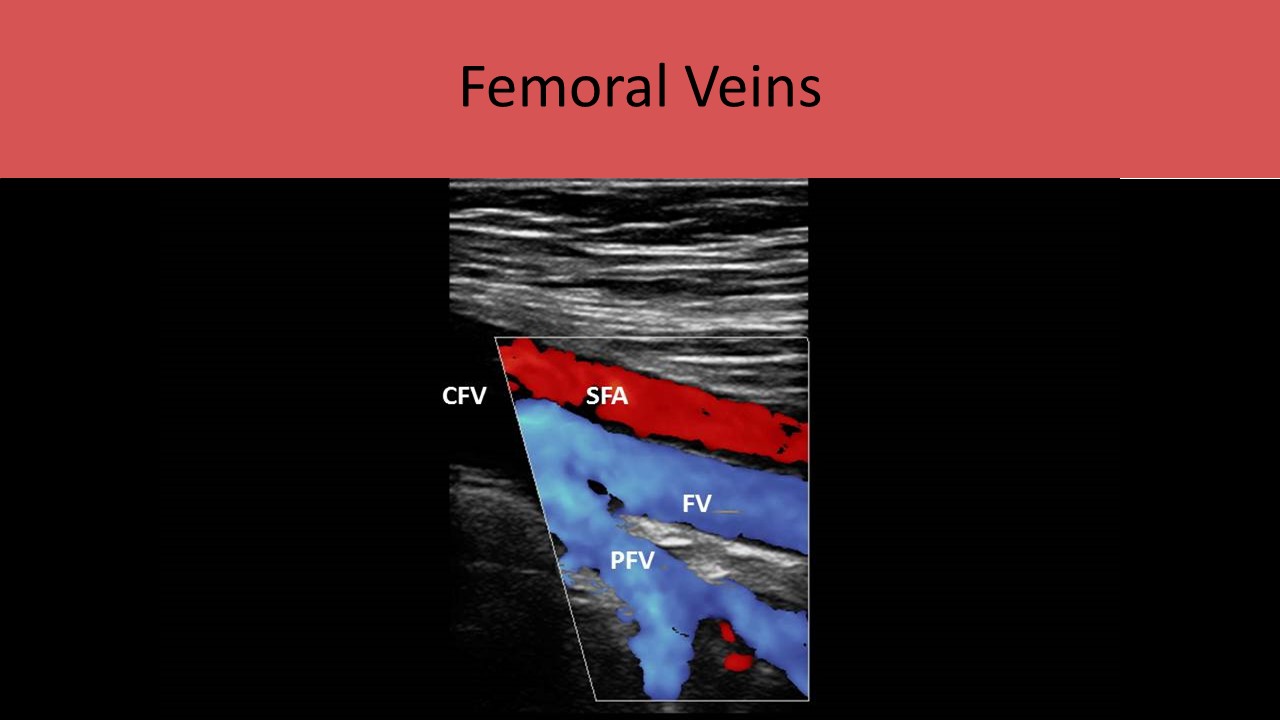
- AKA superficial femoral vein (SFV); nomenclature recommendations remove the term superficial to alleviate confusion regarding this deep vein
- Extends from adductor hiatus to join the profunda femoral vein at the groin
- Courses posterior to the femoral artery
- AKA deep femoral vein (DFV); nomenclature recommendations remove the terms superficial and deep to alleviate confusion regarding both of these veins being part of the deep venous system
- Joins the femoral vein to form the common femoral vein just below inguinal ligament
- Drains the muscles in the thigh (quadriceps)
- Formed by the junction of the FV and PFV, just below the inguinal ligament
- Courses beneath the inguinal ligament
- Becomes external iliac vein just above inguinal ligament at the groin crease
- Courses medial and posterior to common femoral artery
- Courses medial to the external iliac vein
- Drains the pelvic organs (NOT the gonads)
- Courses lateral to the internal iliac vein and anterior to the external iliac artery
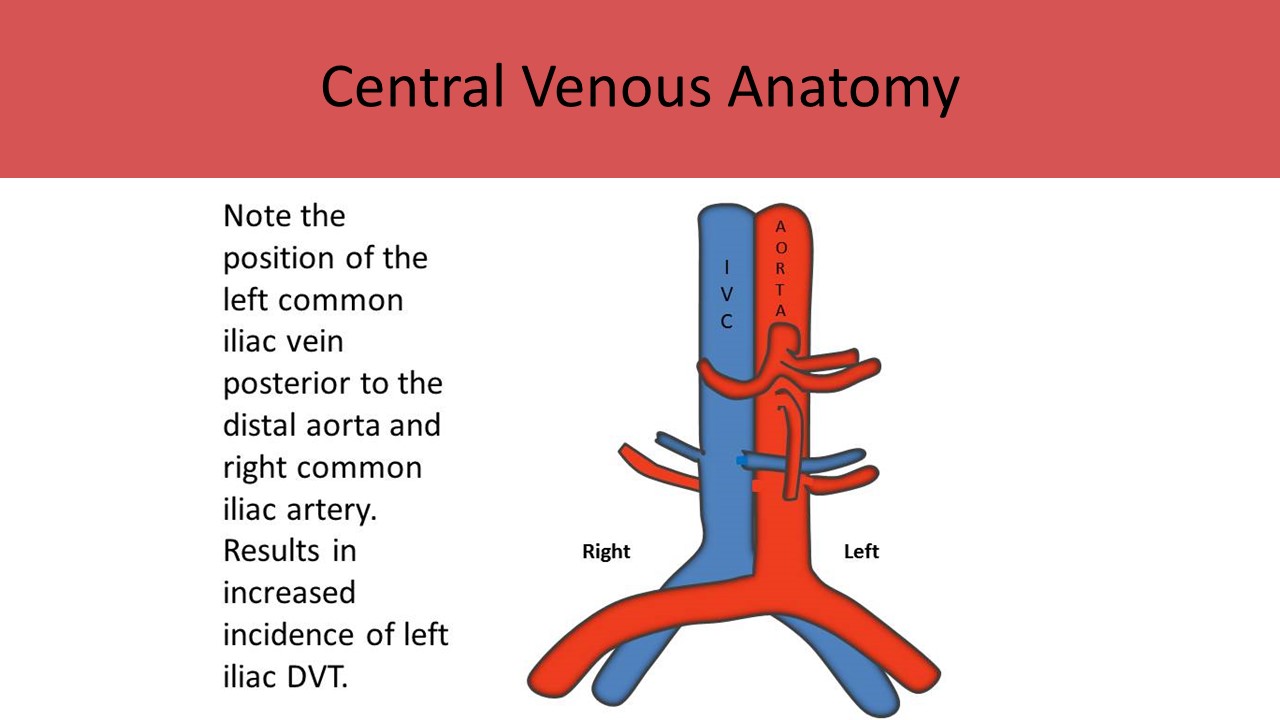
- Joins the internal iliac vein to form the common iliac vein
- Courses anterior to the common iliac artery
- Right and left common iliac veins merge at the level of L5 to form the IVC
- IVC empties into the right atrium
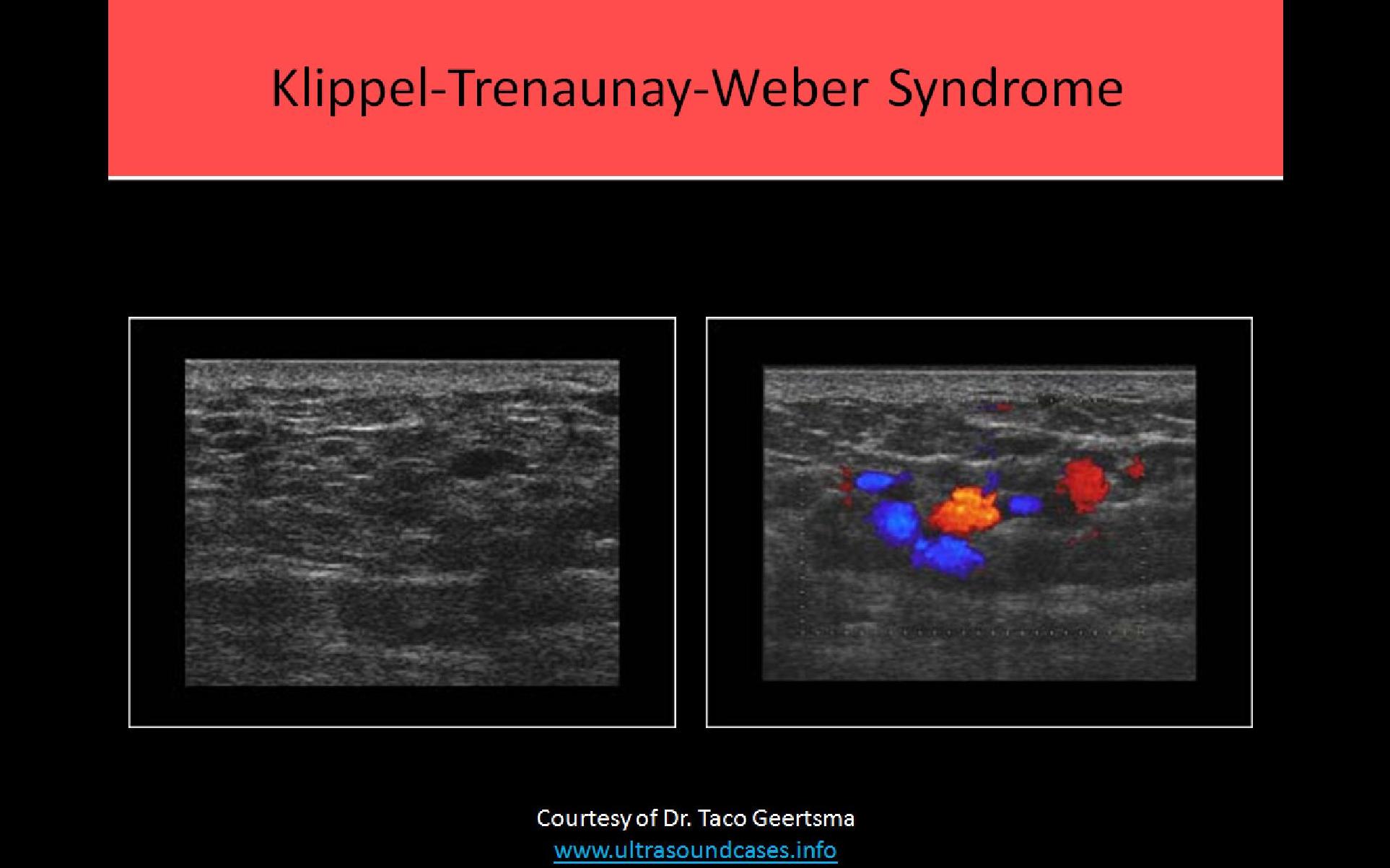
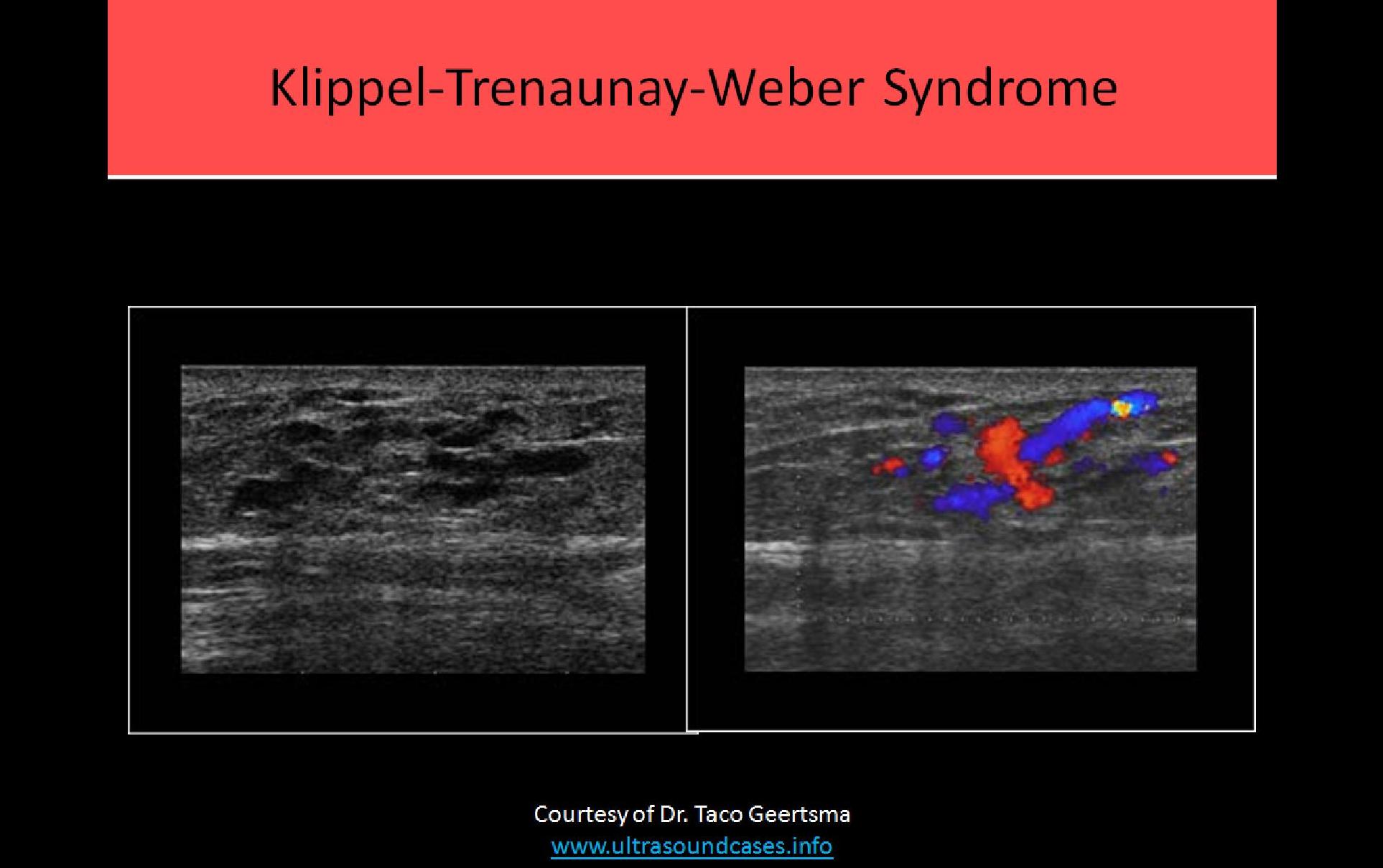
Klippel - Trenaunay - Weber Syndrome:
- Congenital absence of the deep veins
- Causes numerous superficial varicosities and clusters of varicosities
Lower Extremity Superficial Veins:
- Located within 2cm of the skin surface
- Course within the subcutaneous fat layer of the leg
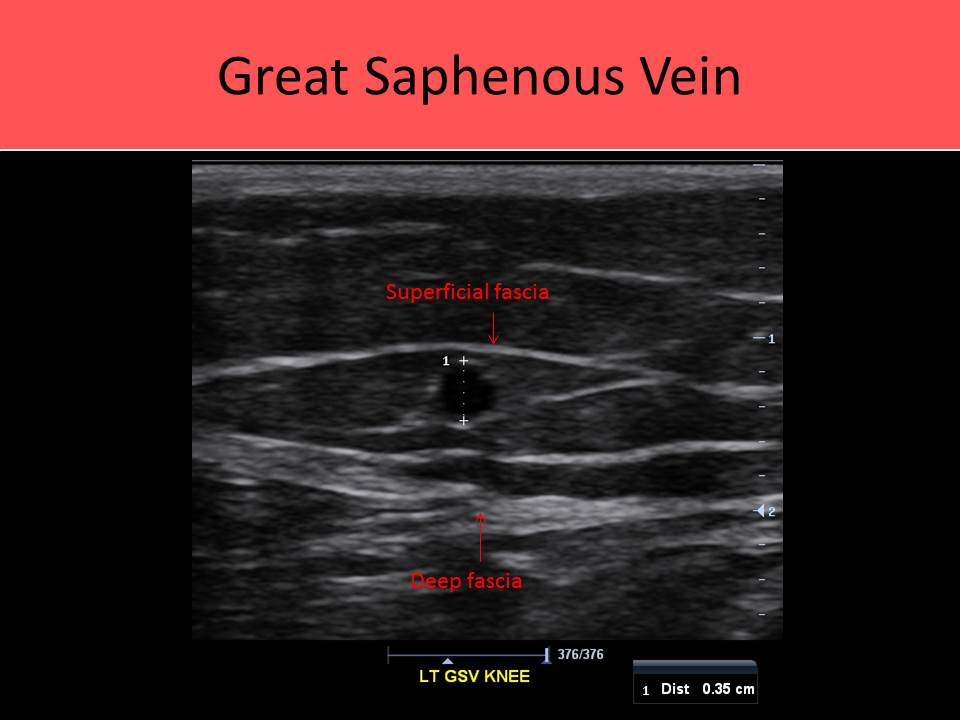
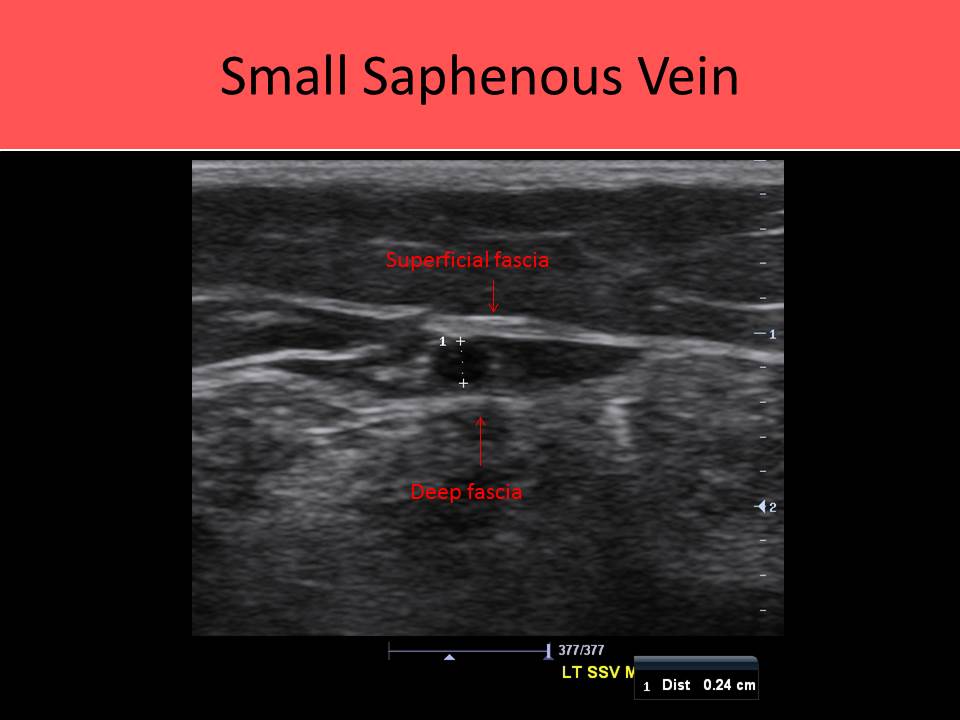
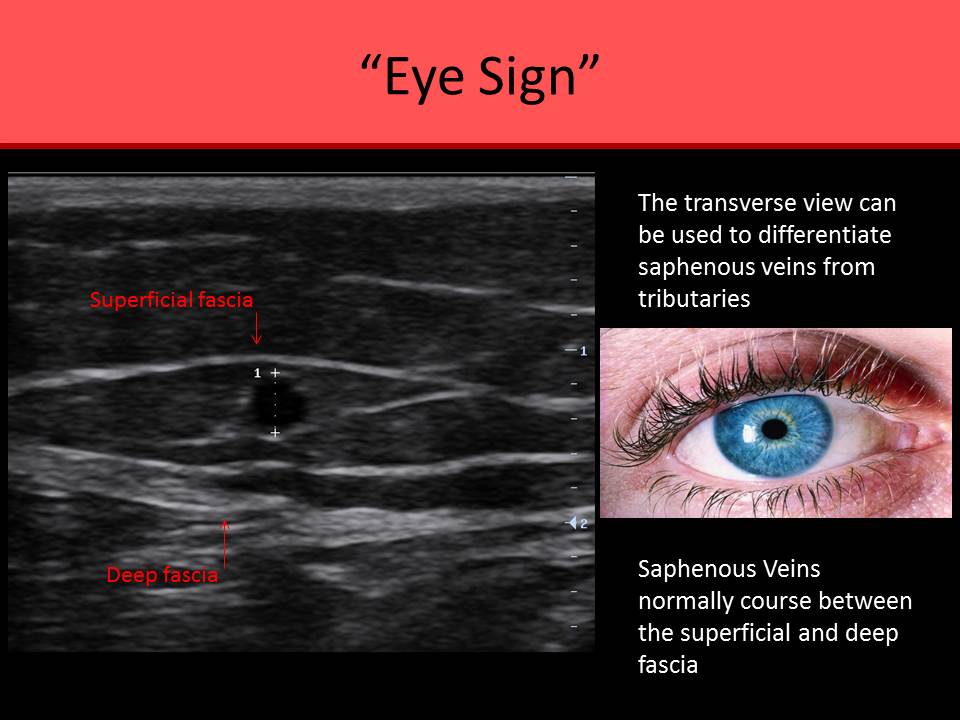
- Veins of the superficial system always course between the superficial and deep fascial layers; use this characteristic location to differentiate from dilated tributaries of the superficial system
Great Saphenous Vein (GSV):
- Longest vein in the body
- Originates on the dorsum of the foot at the medial end of the distal venous arch
- Travels anterior to the medial malleolus
- Ascends medial thigh with the great saphenous nerve
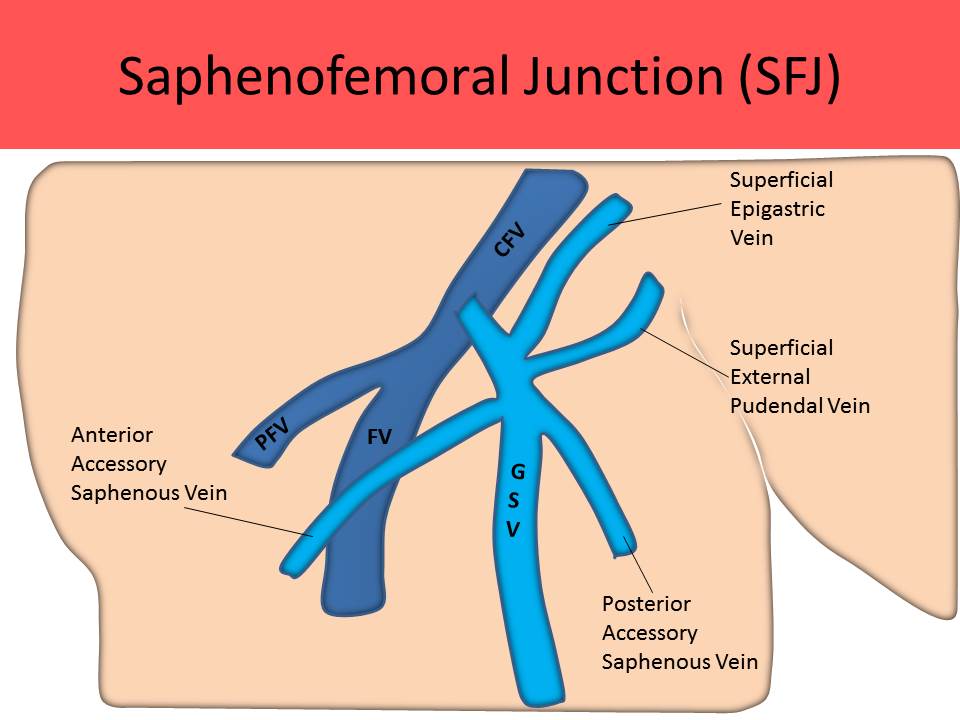
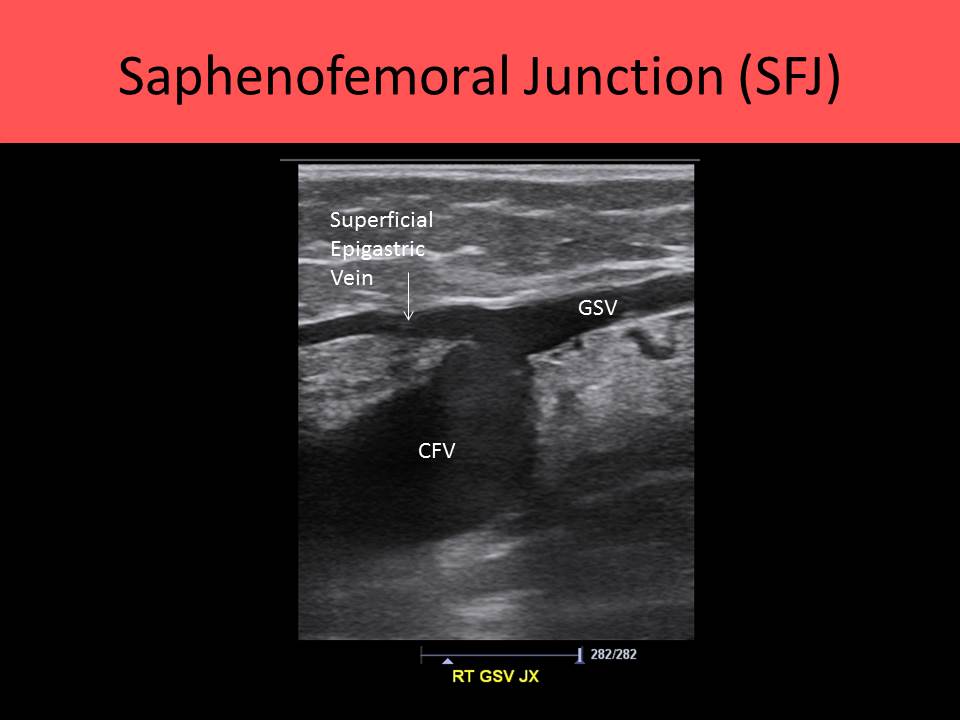
- Penetrates the deep fascia through the foramen ovale in the groin and terminates the saphenofemoral junction
- Saphenofemoral junction (SFJ) is adjacent to the inguinal ligament
- Also connects to deep system through multiple perforating veins
- Superficial epigastric vein is the most proximal tributary of the GSV and usually descends into groin to join the GSV near the saphenofemoral junction
- Commonly used as a bypass graft for cardiac and arterial bypass surgery
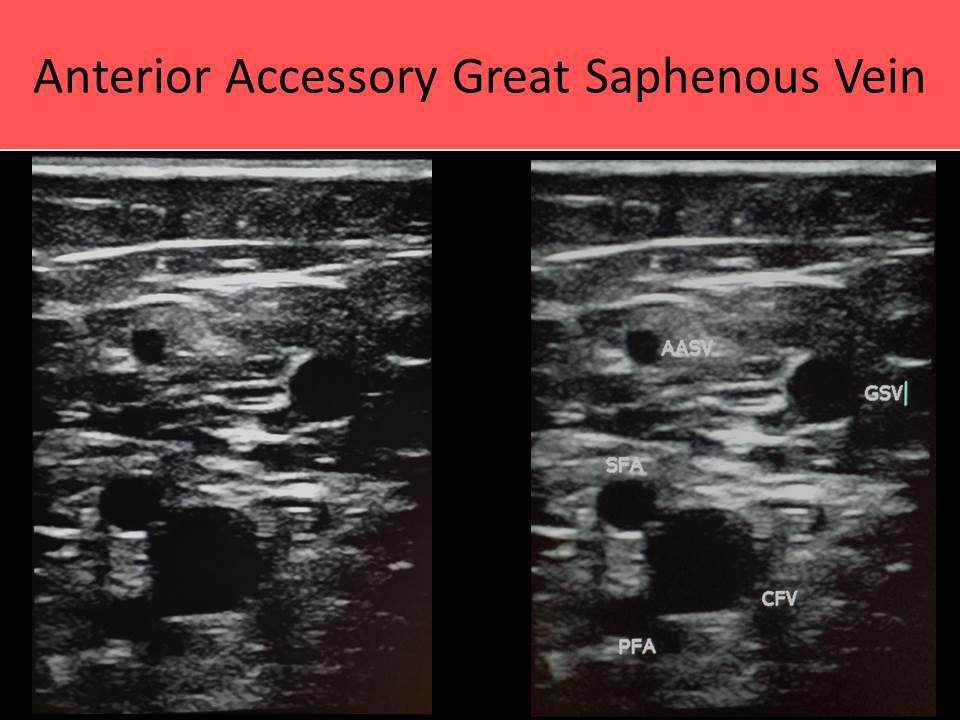
Anterior Accessory Saphenous Vein (AASV):
- Most easily identified at the groin
- Ascends along the thigh to join the GSV near the groin
- Differentiated from the GSV by its course anterior to the femoral artery instead of medial to it (GSV)
- Not visible in all patients; can be a sign of dilated superficial system and reflux
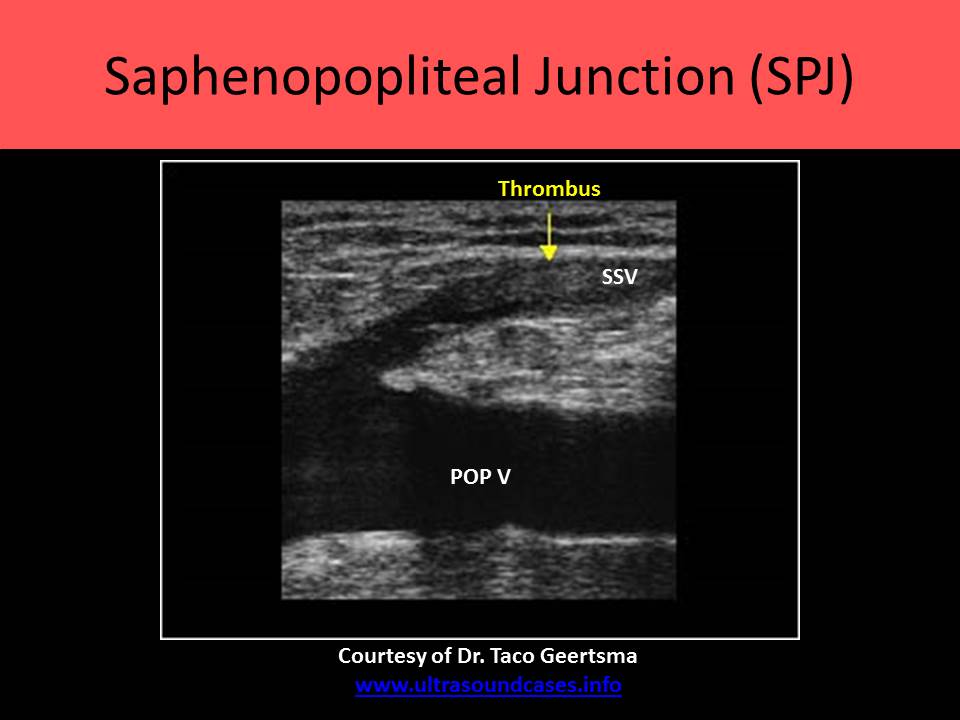
- AKA short saphenous vein
- Dorsal vein of the little toe joins the lateral end of the dorsal venous arch to form the SSV
- Originates posterior to lateral malleolus and Achilles tendon
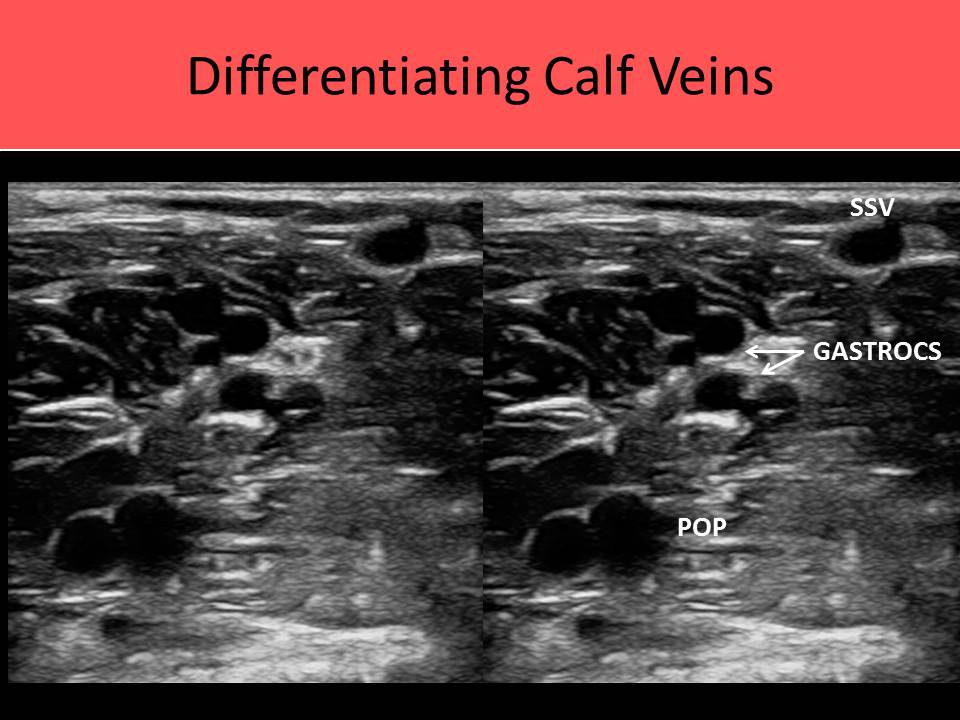
- Ascends along the midline aspect of posterior calf to enter the popliteal space between the two heads of the gastrocnemius muscles
- Usually joins the popliteal vein in knee/distal thigh area but many variations in termination possible
- Course of the vessel on the posterior calf described as a "stocking seam"
- Numerous small vessels connect the SSV to the GSV in the calf
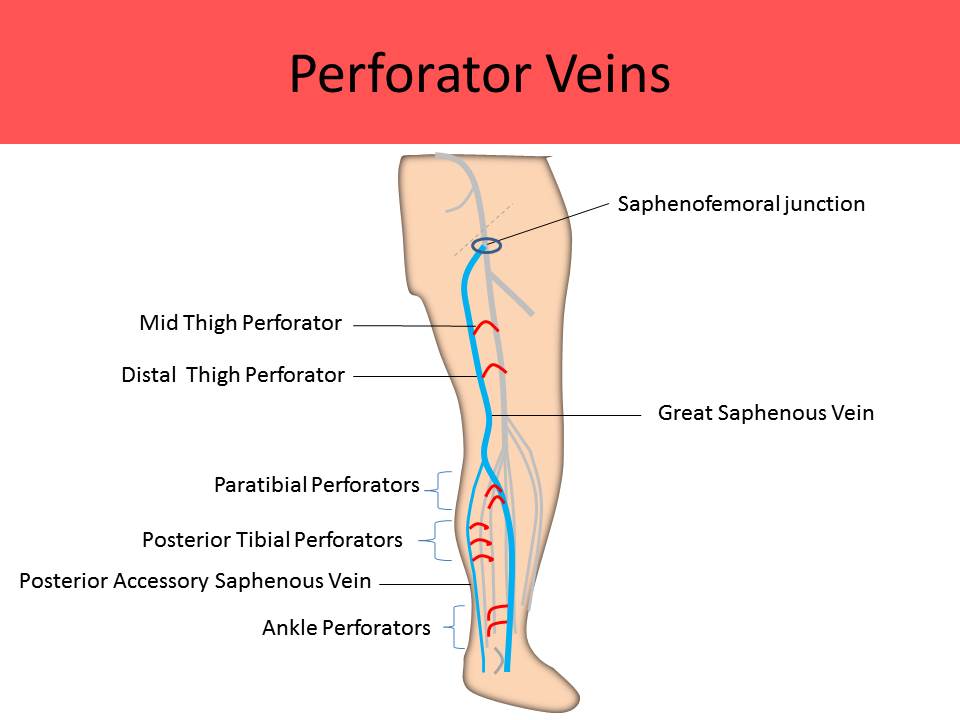
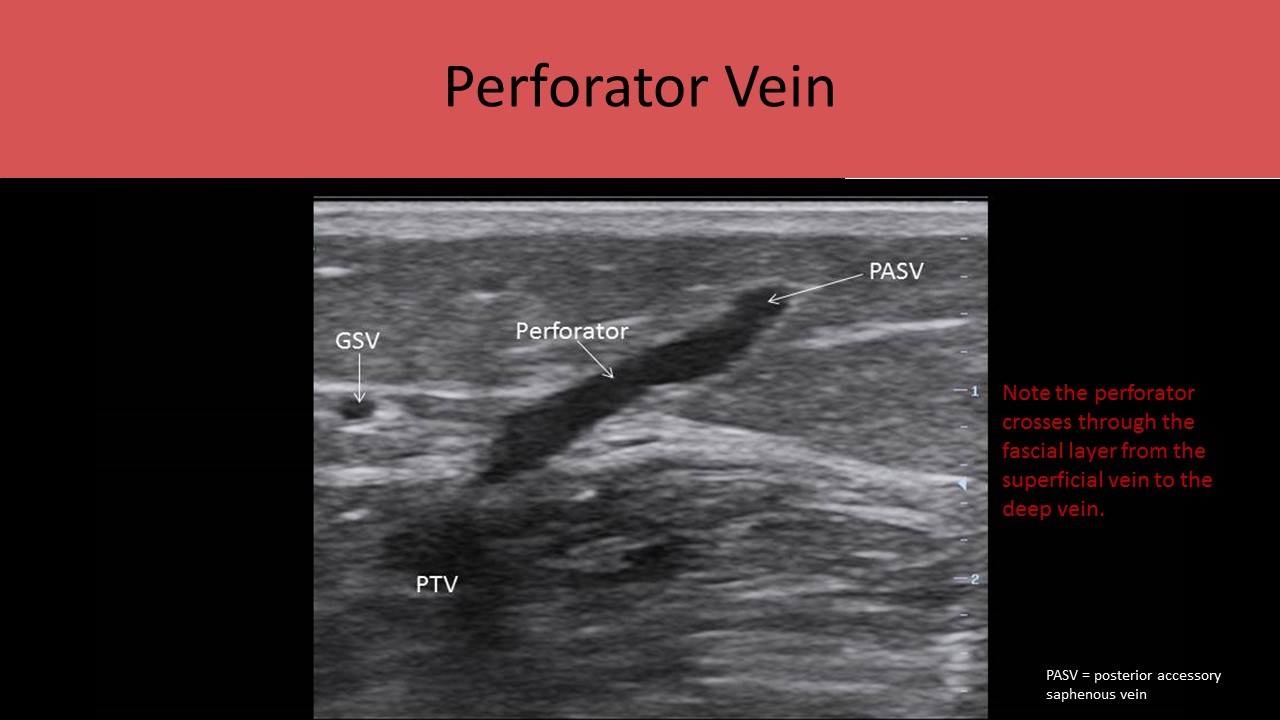
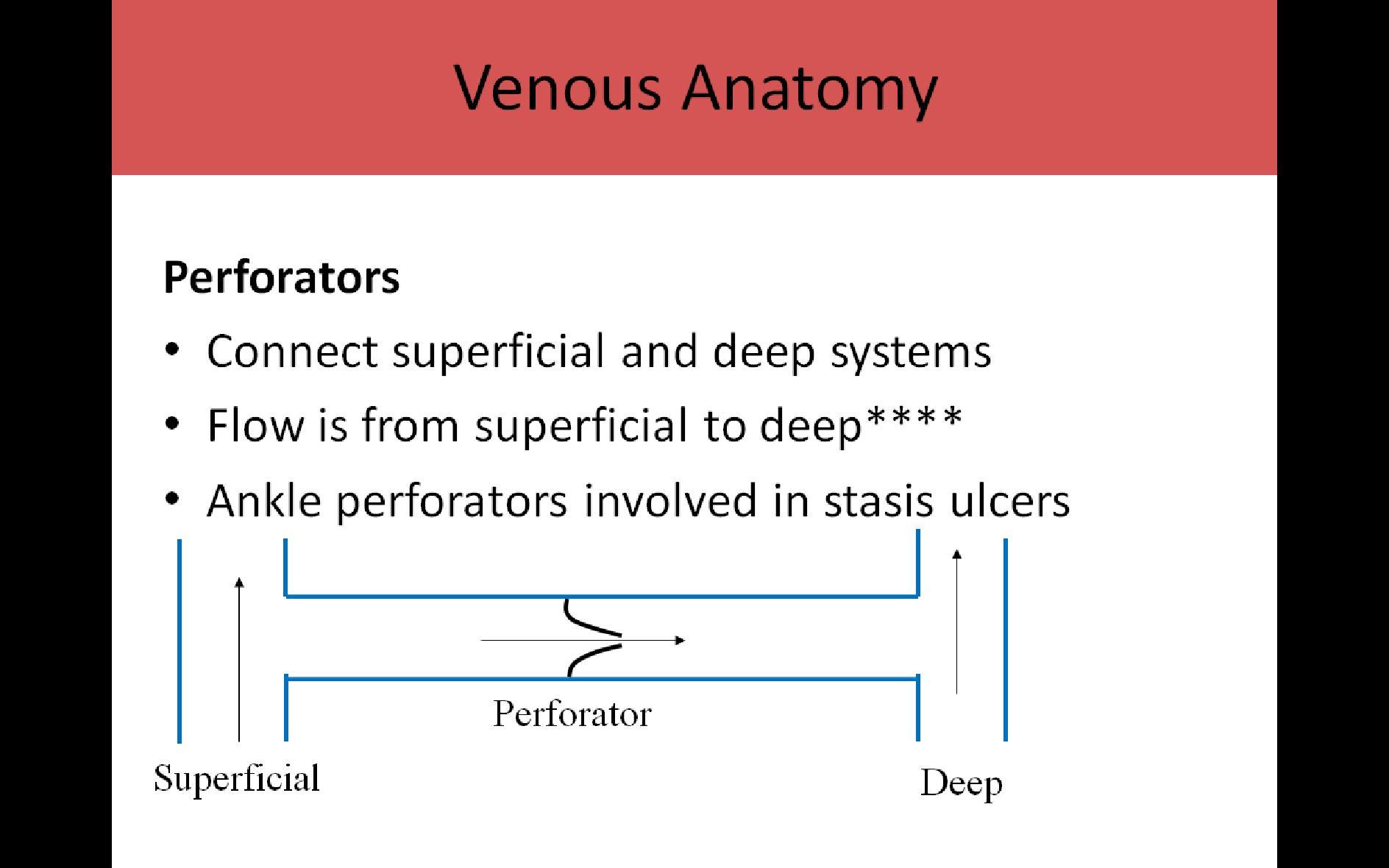
Perforators:
- Connect superficial and deep systems to equalize pressure between the two systems
- Begin in the saphenous compartment and penetrate the deep fascia to join the deep veins
- Normal flow is described as centripetal or from superficial system toward the center of the leg to the deep system
- Each perforator has one valve that allows unilateral flow direction from superficial to deep
- PTV connected to distal GSV near ankle
- 3 ankle perforators called posterior tibial perforators (formerly Crockett's Perforators)
- Paratibial perforators (formerly Boyd's Perforators) located in the knee area; connect GSV to PTVs
- Distal thigh perforators (Dodd's Perforators) located in distal thigh; connect GSV to FV
- Hunterian Perforators located in proximal thigh; connect GSV to FV
- Lateral perforator connects to SSV near the mid calf
- Each leg normally has about 100 perforators
- Normally <2mm diameter, >4mm usually has reflux
- Flow is normally from superficial system to deep system****
- Ankle perforator damage/dilatation involved in stasis ulcers
- Dilated perforators can occur in response to DVT formation
- Connect the great and short saphenous veins
- Never penetrate the deep fascia
- Posterior arch vein extends cephalad from the ankle to join the GSV in the mid calf; communicates with the posterior tibial perforators (Crockett's perforators) and plays a major role in venous stasis ulcers
- Vein of Giacomini originates at the saphenopopliteal junction (SSV/POP) behind the knee and extends up the posterior thigh to become the posterior circumflex vein that joins the GSV

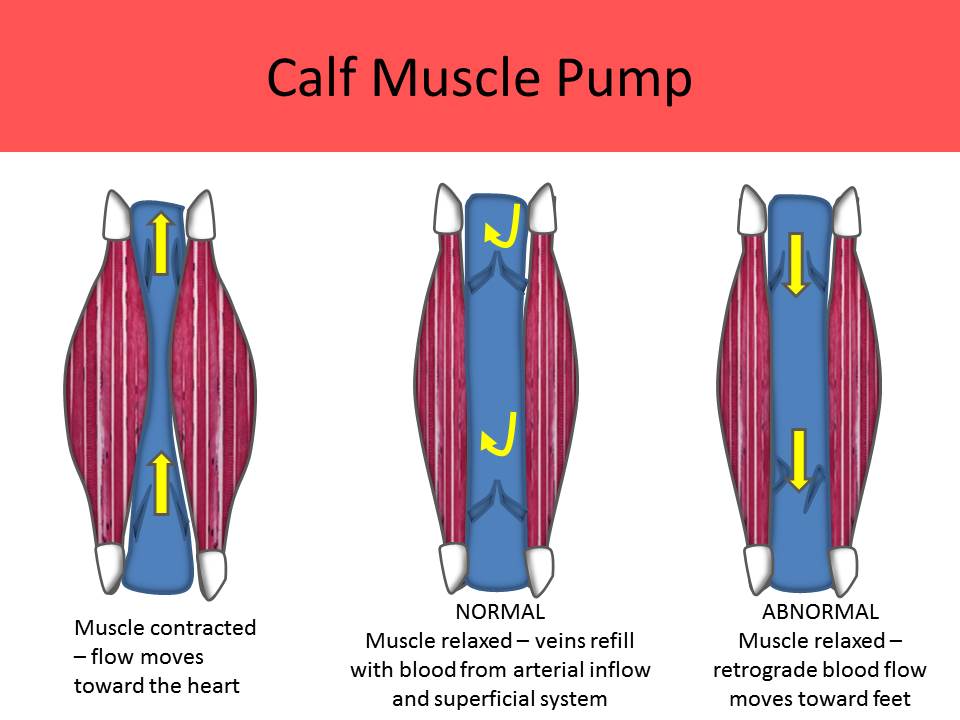
Sural Veins (sinusoid or saccular veins):
- Serve as blood reservoirs for the legs
- Important for calf muscle pump and lower extremity venous flow
- Gastrocnemius Plexus:
- Group of calf veins
- Have an accompanying artery with each set
- Usually seen as two pairs, lateral and medial sets
- May see three pairs
- Most commonly drain into the popliteal vein
- cannot be followed to the ankle and this characteristic can be used to differentiate them from the tibial veins
- Soleal Plexus/Soleal Sinuses:
- Thick walled reservoirs within the soleal muscle
- No artery with them
- Do NOT contain valves
- Drain into either the posterior tibial or peroneal veins
- Most lower extremity DVT starts in these vessels
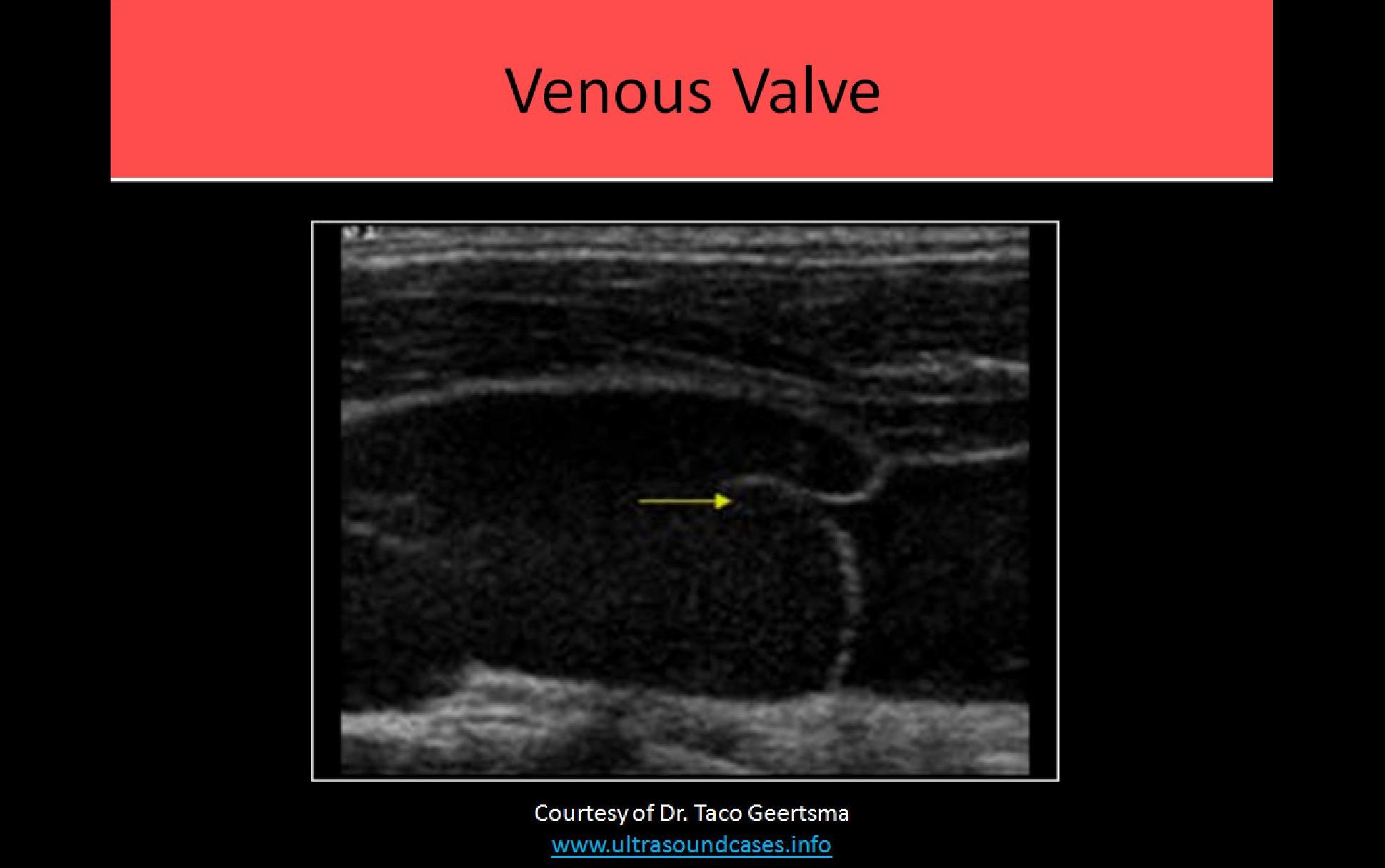
Valves:
- Extensions of the intimal layer
- Valves contain two leaflets (bicuspid)
- Primary purpose is to allow unilateral flow direction in veins
- Helps keep flow moving from superficial to deep system and from peripheral to deep veins
- The GSV has the most valves because it is the longest vein in the body and it is located outside the muscle tissue
- Each perforating vein has a single valve

Available products and price list on next page
| Return to Top | Reference List |