
.jpg)
Valvular Abnormalities and Disease
Primary vs. Secondary Findings:
A primary finding refers to the primary cause of the abnormality EX: atherosclerosis formation on the aortic valve causes the stenosis
A secondary finding refers to other abnormalities caused by the primary abnormality EX: aortic stenosis causes thickening of the LV wall and post-stenotic dilatation of the aortic root
Four Considerations When Evaluating Cardiac Valves:
- How many valve leaflets are present?
- Do you see abnormal masses, thickening or calcification attached to the valve leaflets?
- Is leaflet mobility normal, restricted or hypermobile?
- What are the associated abnormalities of the cardiac chambers and other cardiac valves?
AORTIC VALVE ABNORMALITIES
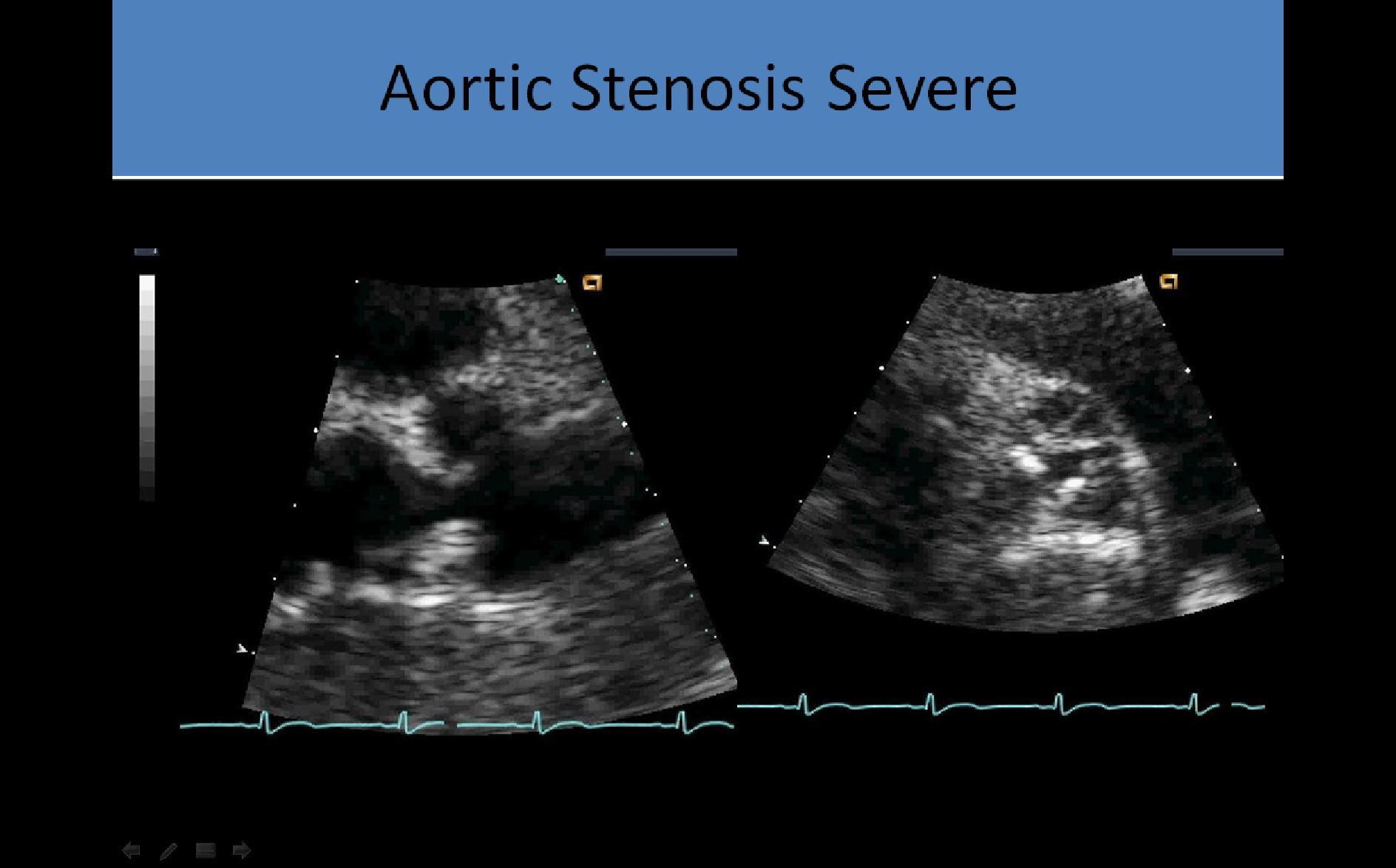
Aortic Stenosis - Atherosclerosis:
- Varying degrees of leaflet thickening will be demonstrated
- Fusion of the edges of the leaflets may occur with severe stenosis
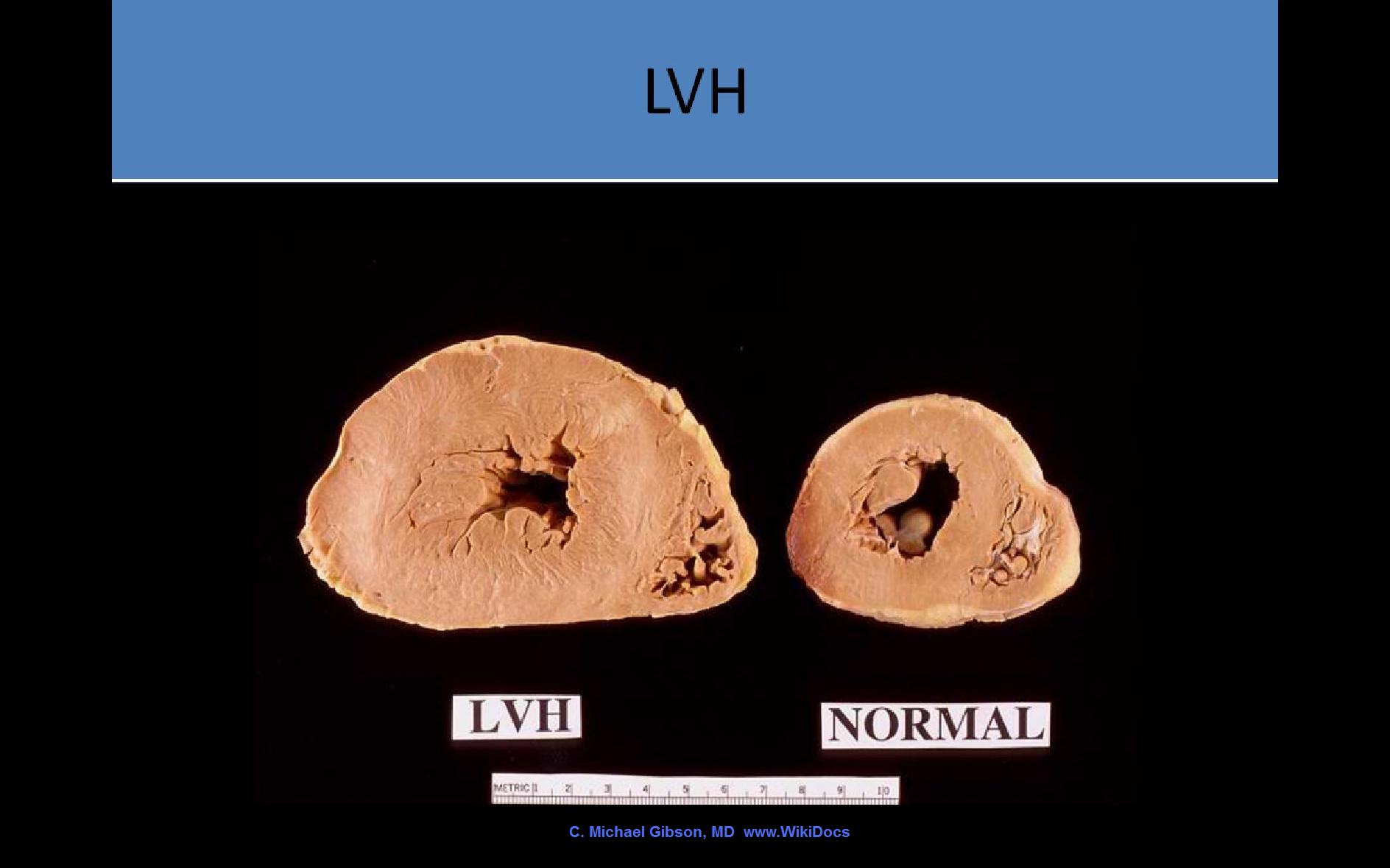
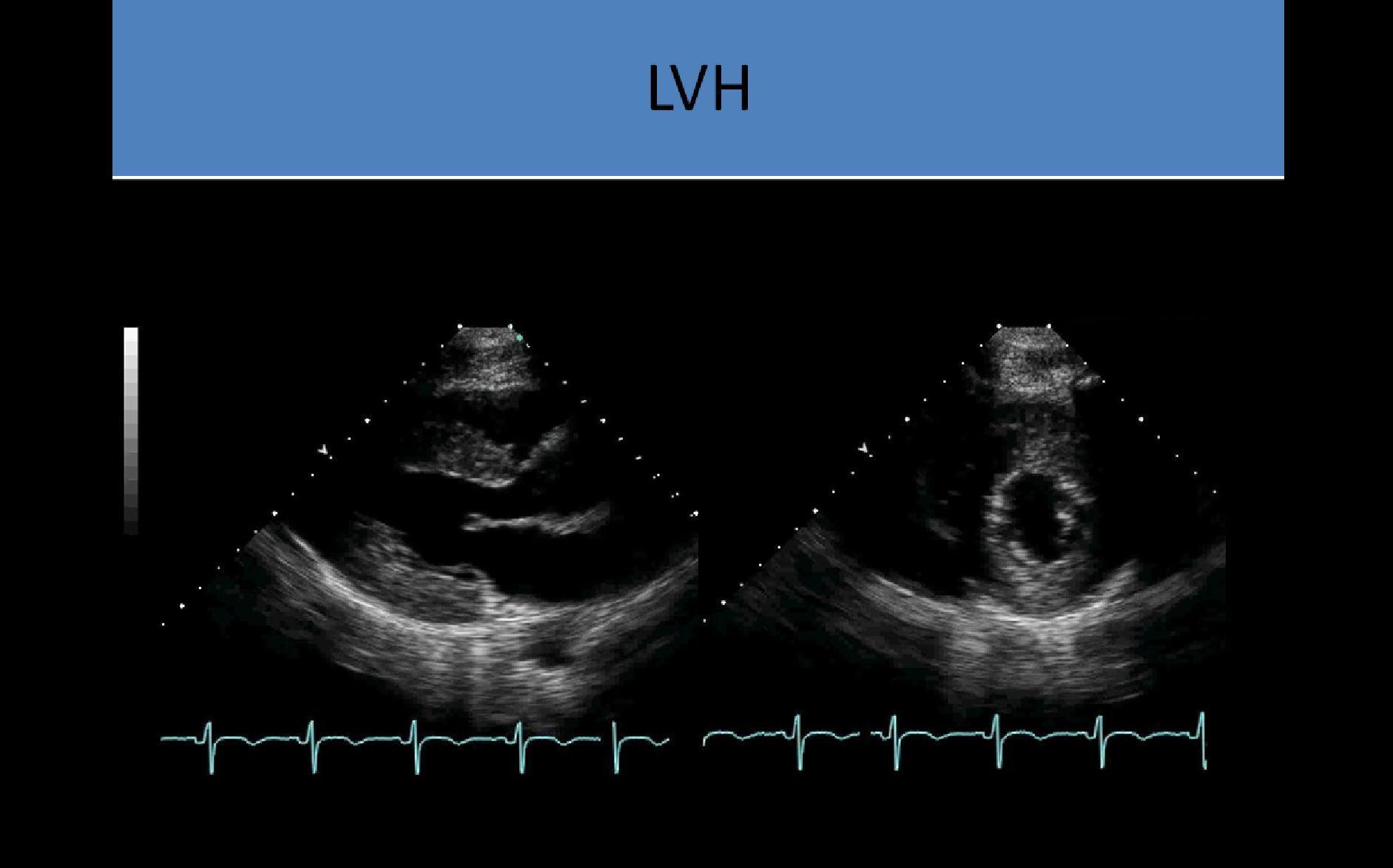
- Hypertrophy of the muscle wall of the ventricle will occur as it adapts to the chronic pressure overload
Clinical Symptoms:
- Dyspnea/Shortness of breath most common symptom
- Orthopnea
- Palpitations
- Fatigue
- Dizziness and syncope due to decreased cardiac output
- Harsh systolic crescendo-decrescendo murmur best heard at the right upper sternal border
- Systolic ejection click
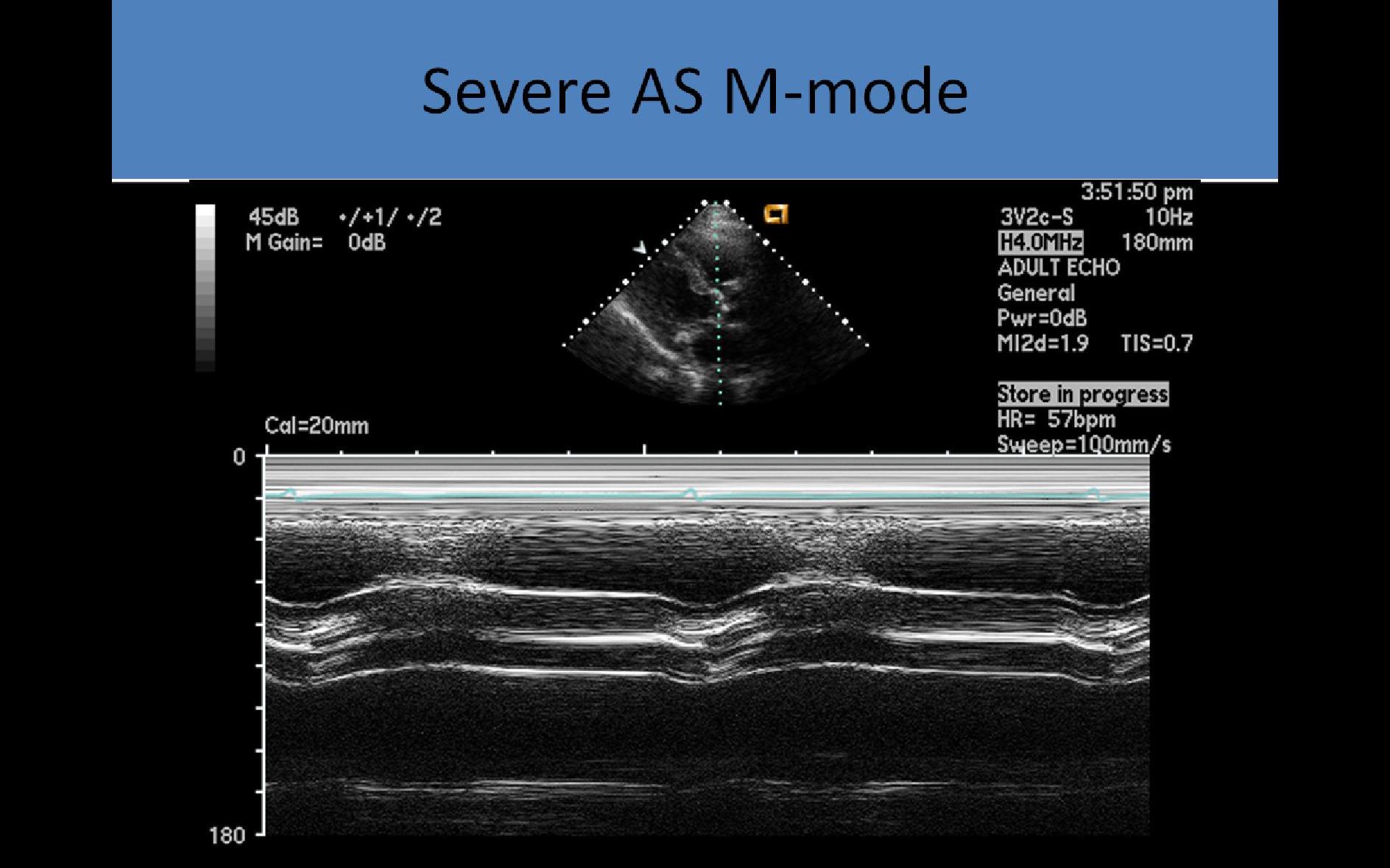
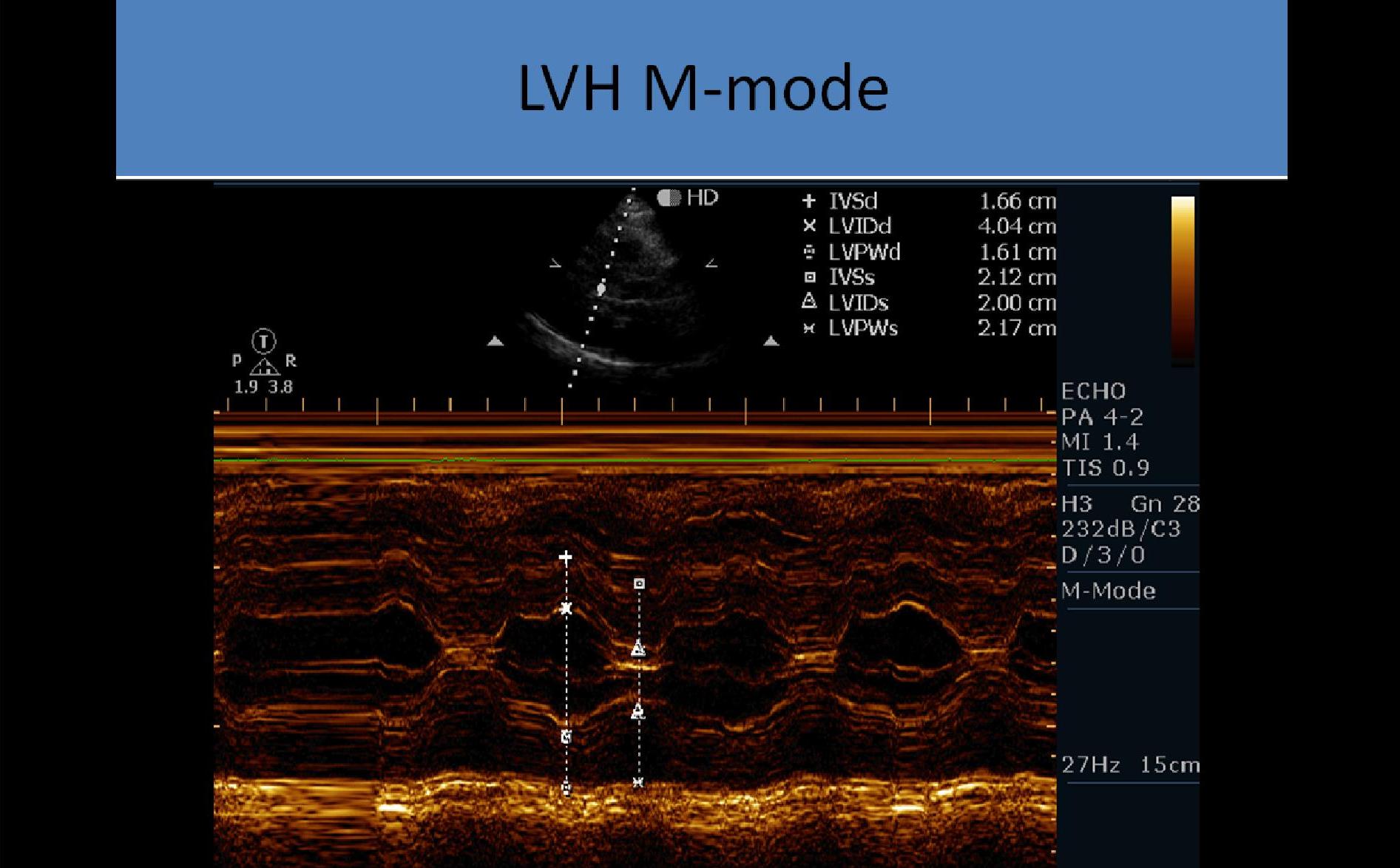
M-mode:
- Used to assess systolic leaflet separation
- <12 mm cusp separation indicates significant obstruction
- Method is not very accurate in determining the severity of the stenosis
- Thickened leaflets cause multiple echoes to be displayed in diastole
- Decreased leaflet separation and multiple echoes filling the space between the aortic root and AV opening
- LVH due to pressure overload
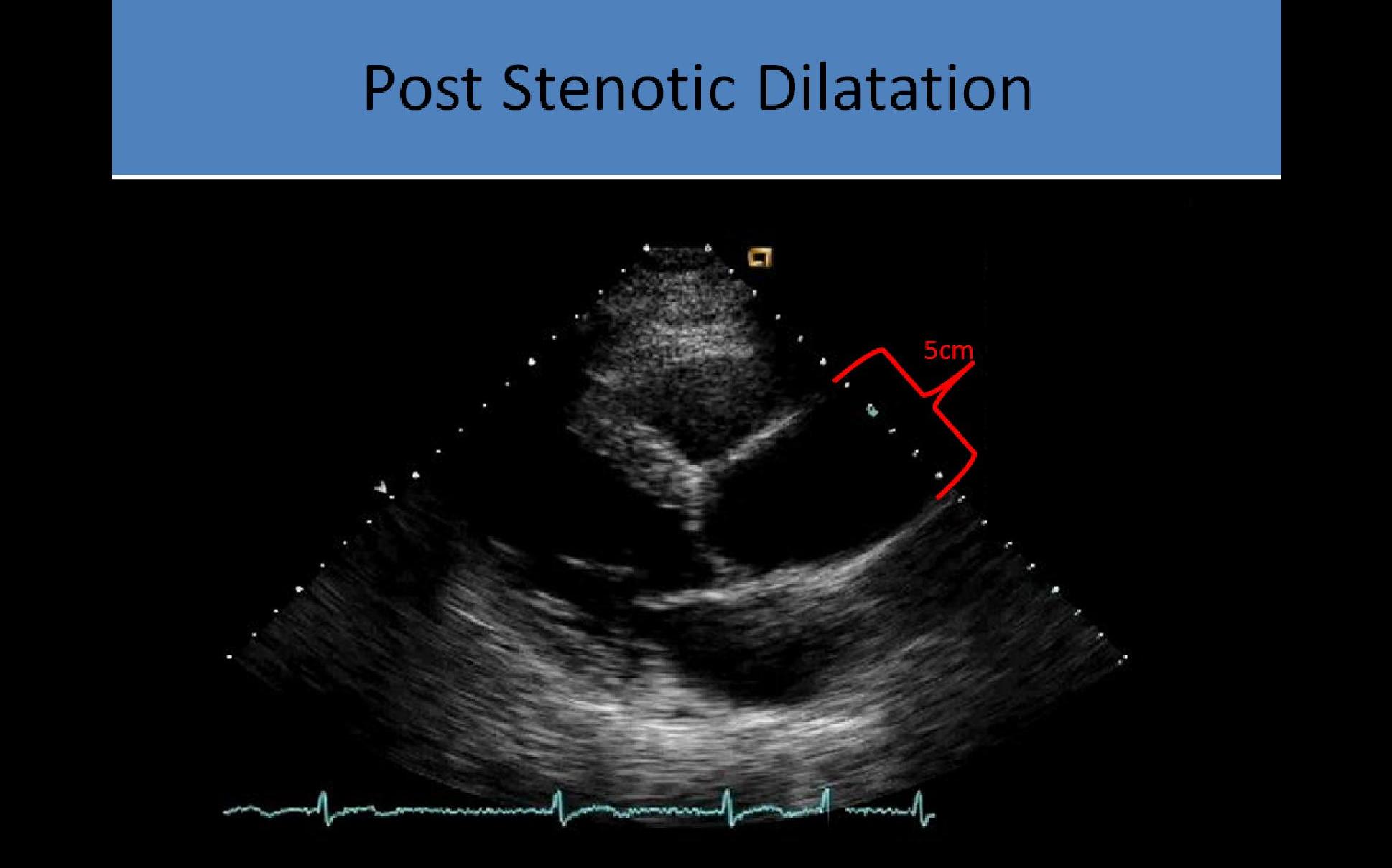
- Post stenotic aortic root dilatation due to eccentric flow through stenosis
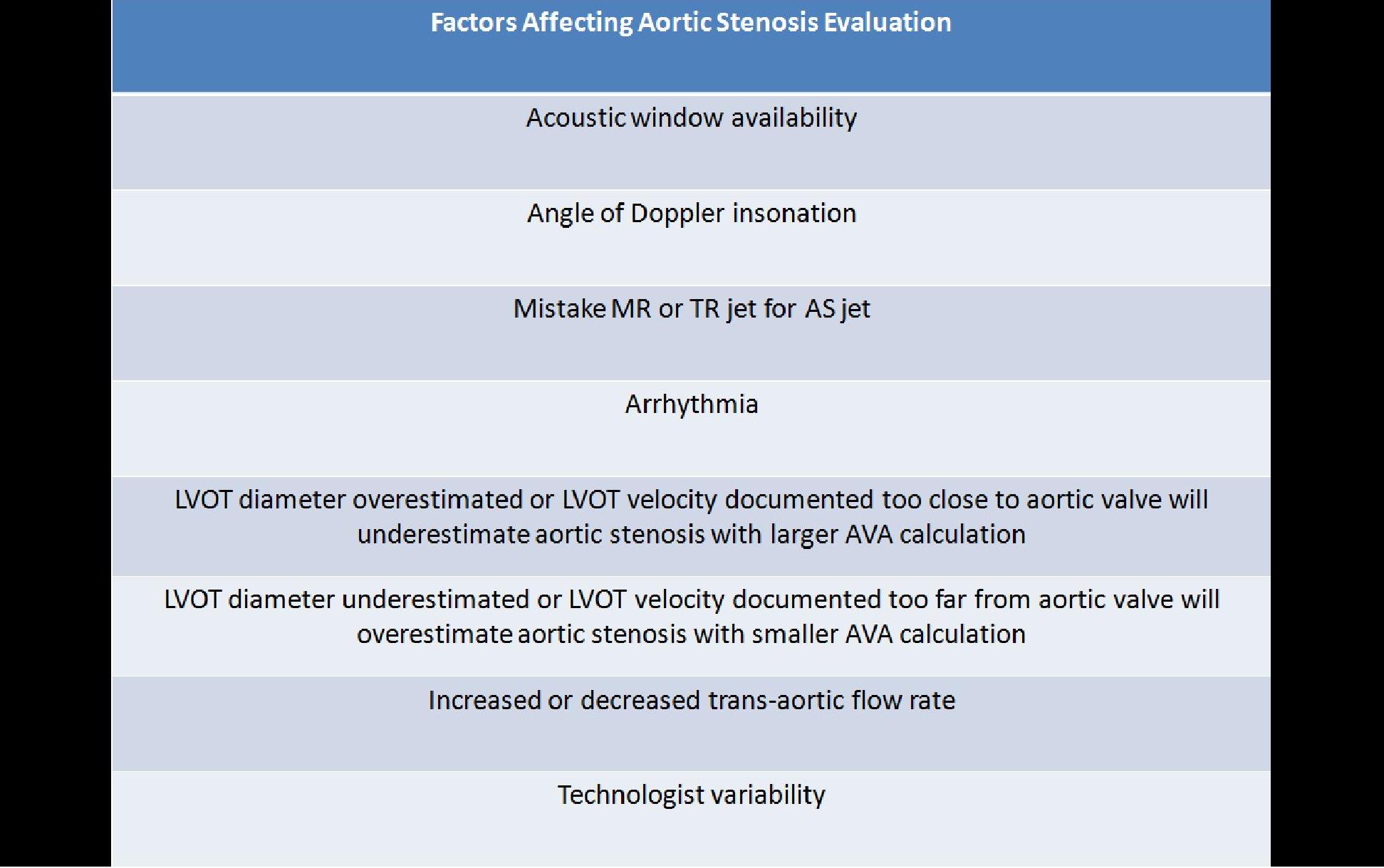
2D and Doppler Evaluation:
- PLAX - delineates the restricted opening of the tips of the aortic leaflets
- PSAX - at the level of the aortic valve demonstrates the true orifice of the stenotic valve ; area can be traced, ****planimetry is not very accurate because heavily calcified leaflets cause bright echoes with poorly defined borders making measurement difficult
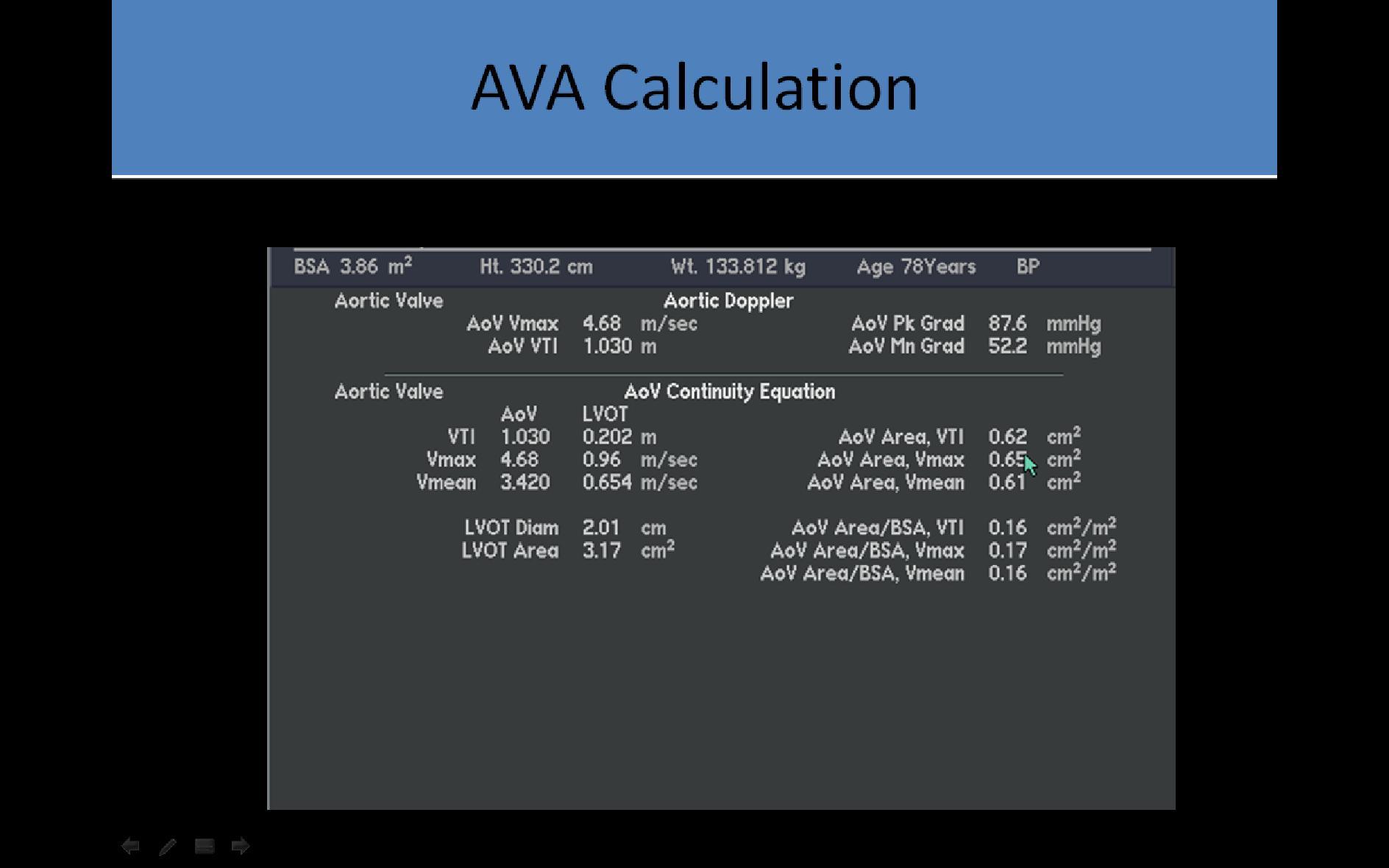
- AP 5/AP 3 – Doppler evaluation of the LVOT and AV velocities
- Pedoff probe applied at the apical, right parasternal and suprasternal windows
- Average normal aortic valve area is 3cm2
- Average PSV 1.4m/s
- Increasing velocities and acceleration times are noted with increasing severity of stenosis
- Aortic flow may be recorded from the apical, suprasternal or parasternal locations
- Velocity and PPG alone cannot diagnose stenosis due to variations in cardiac output, you must know the valve area
- Heavy calcification on the leaflets can lead to understimation of stenosis due to degraded Doppler signal and inability to locate the highest velocity
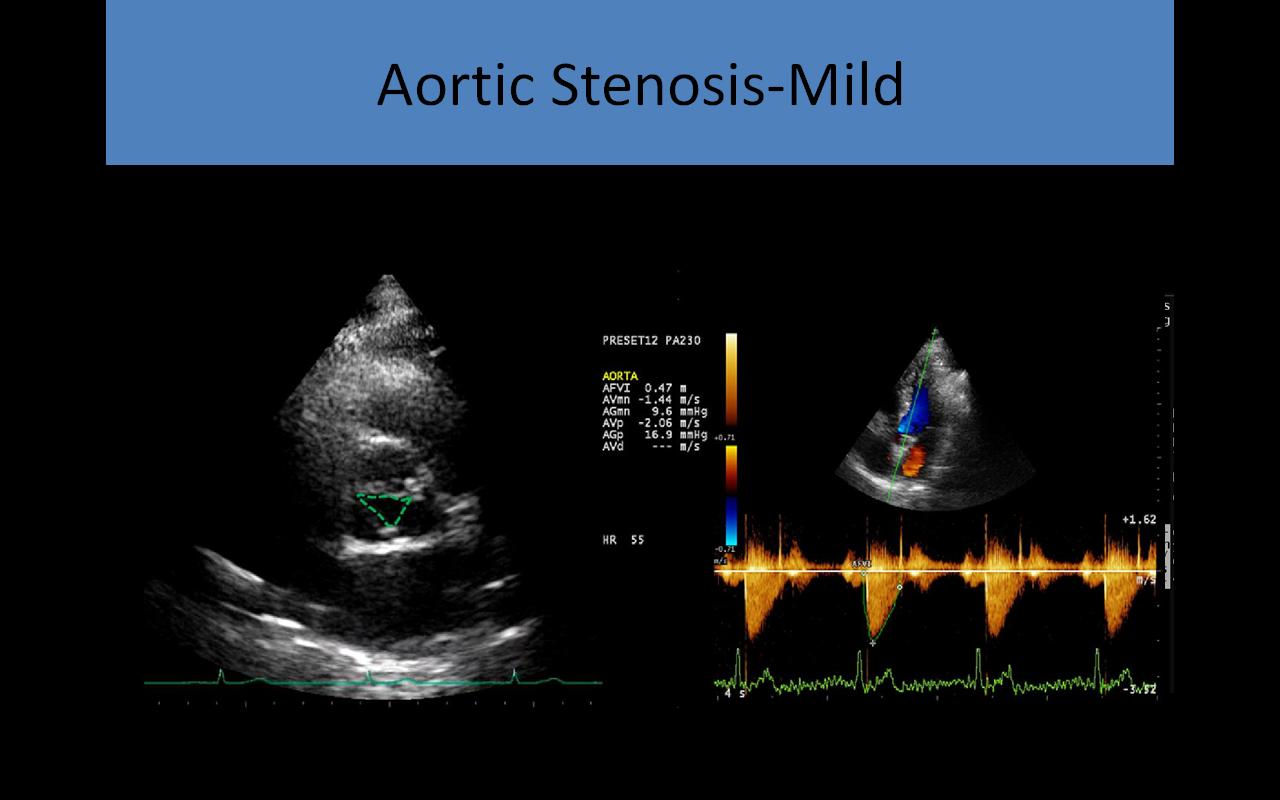
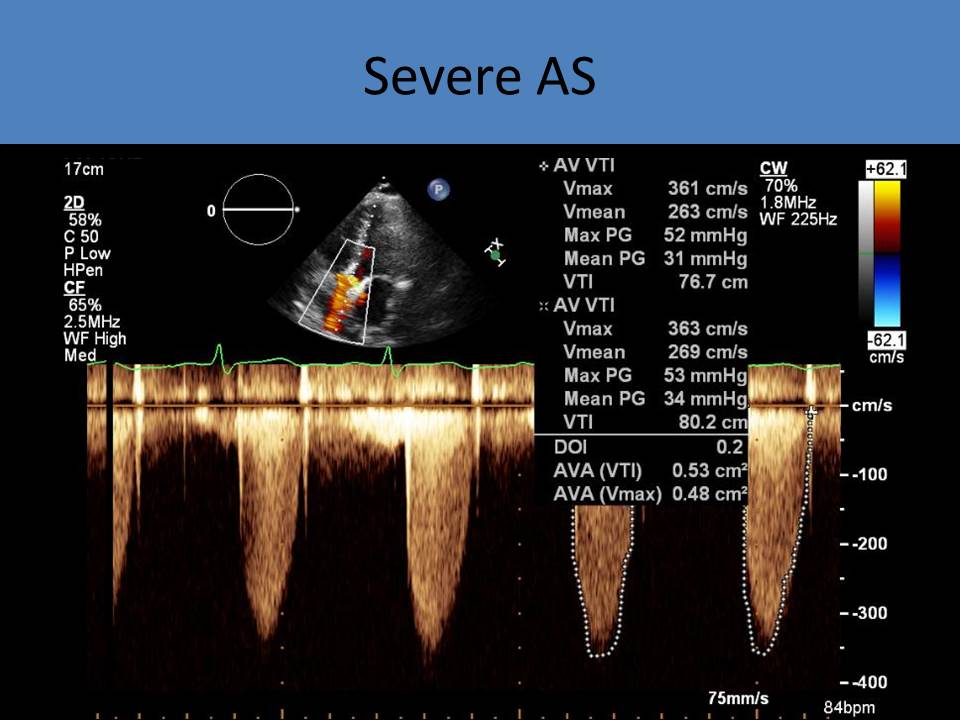
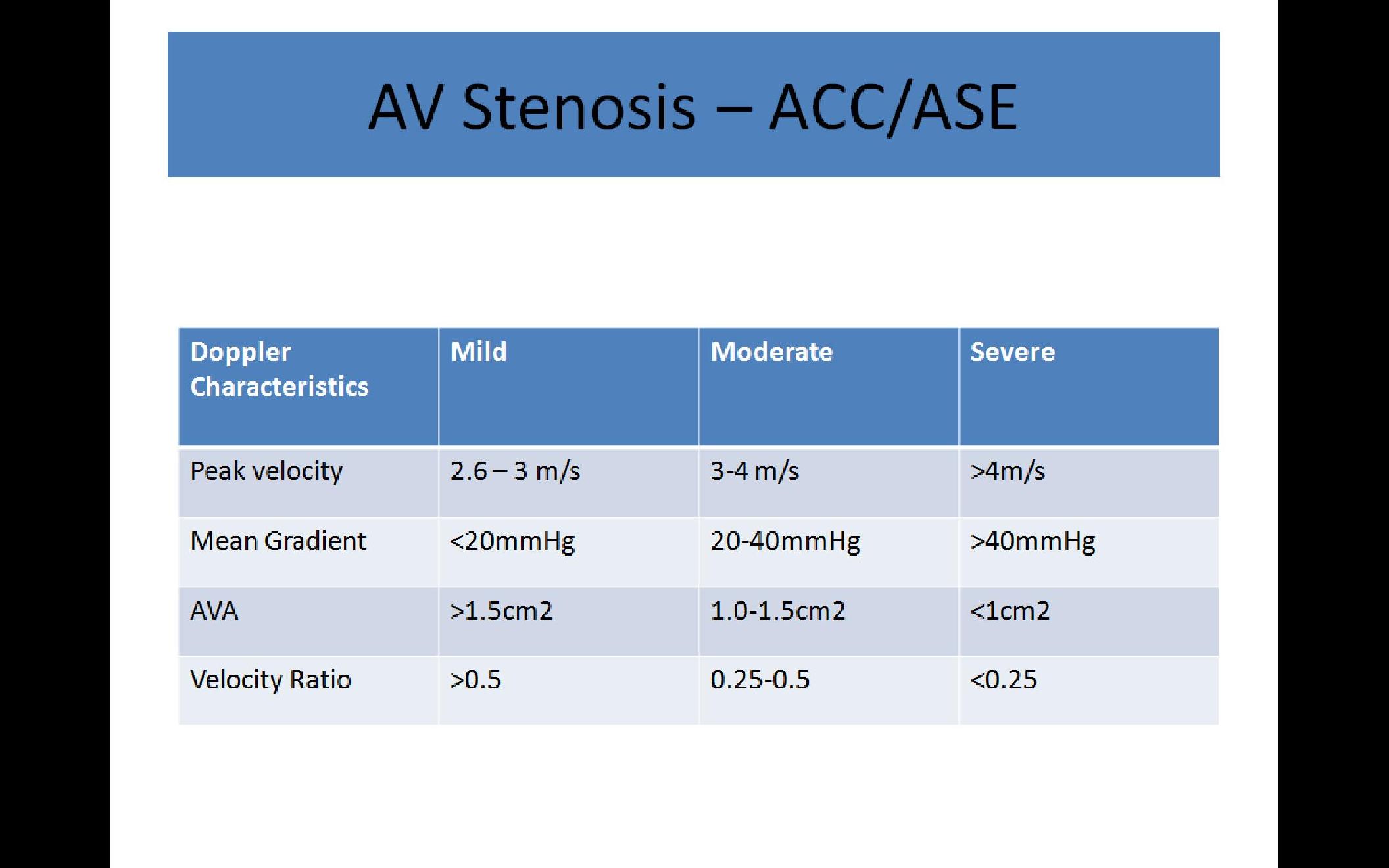
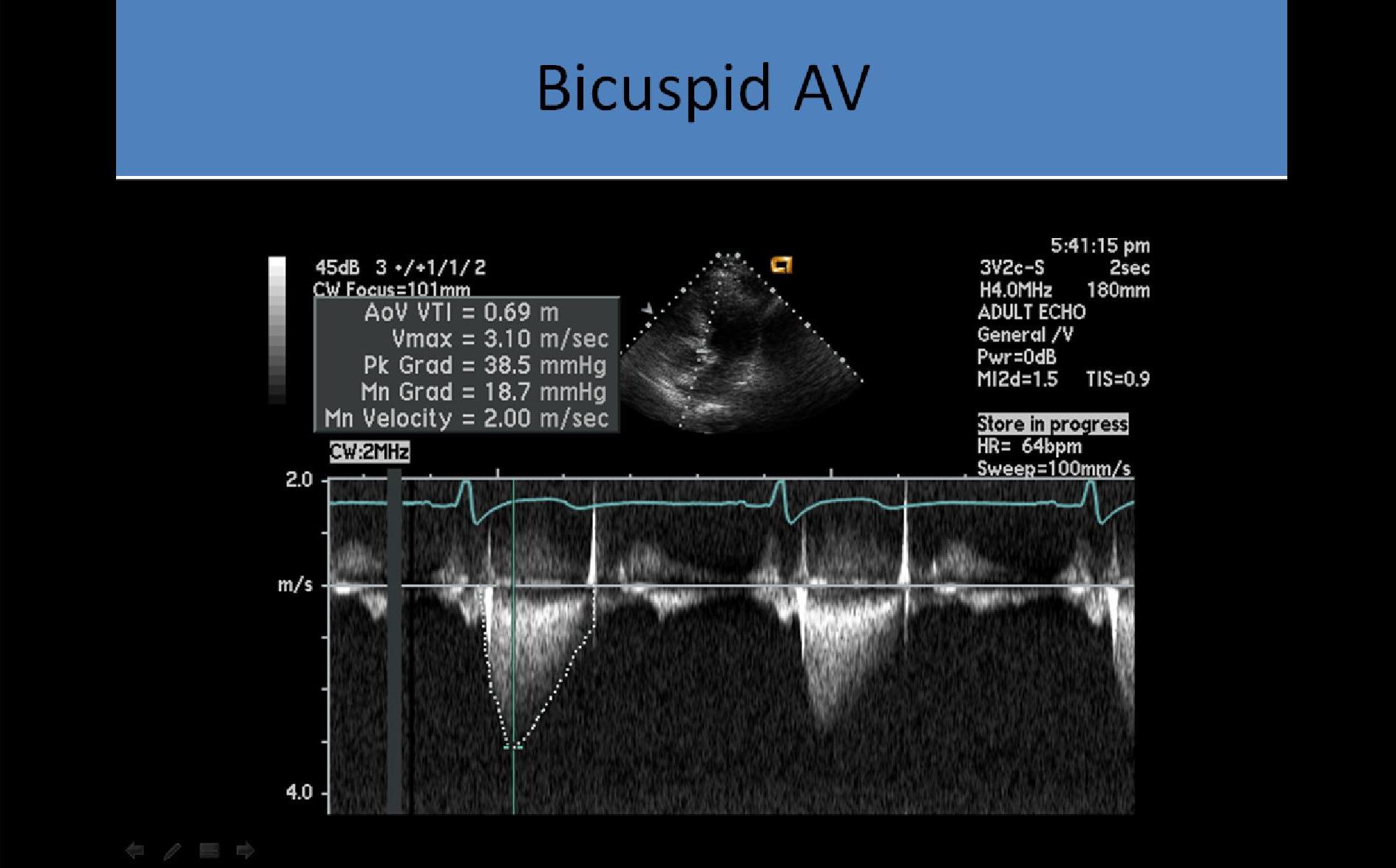
ASE Classifications:
- Aortic sclerosis <2.5m/s
- Mild: PSV 2.6 – 3m/s; PPG <36mmHg
- Moderate: PSV 3 – 4m/s; PPG 36 – 64mmHg
- Severe: PSV >4m/s; PPG >64mmHg
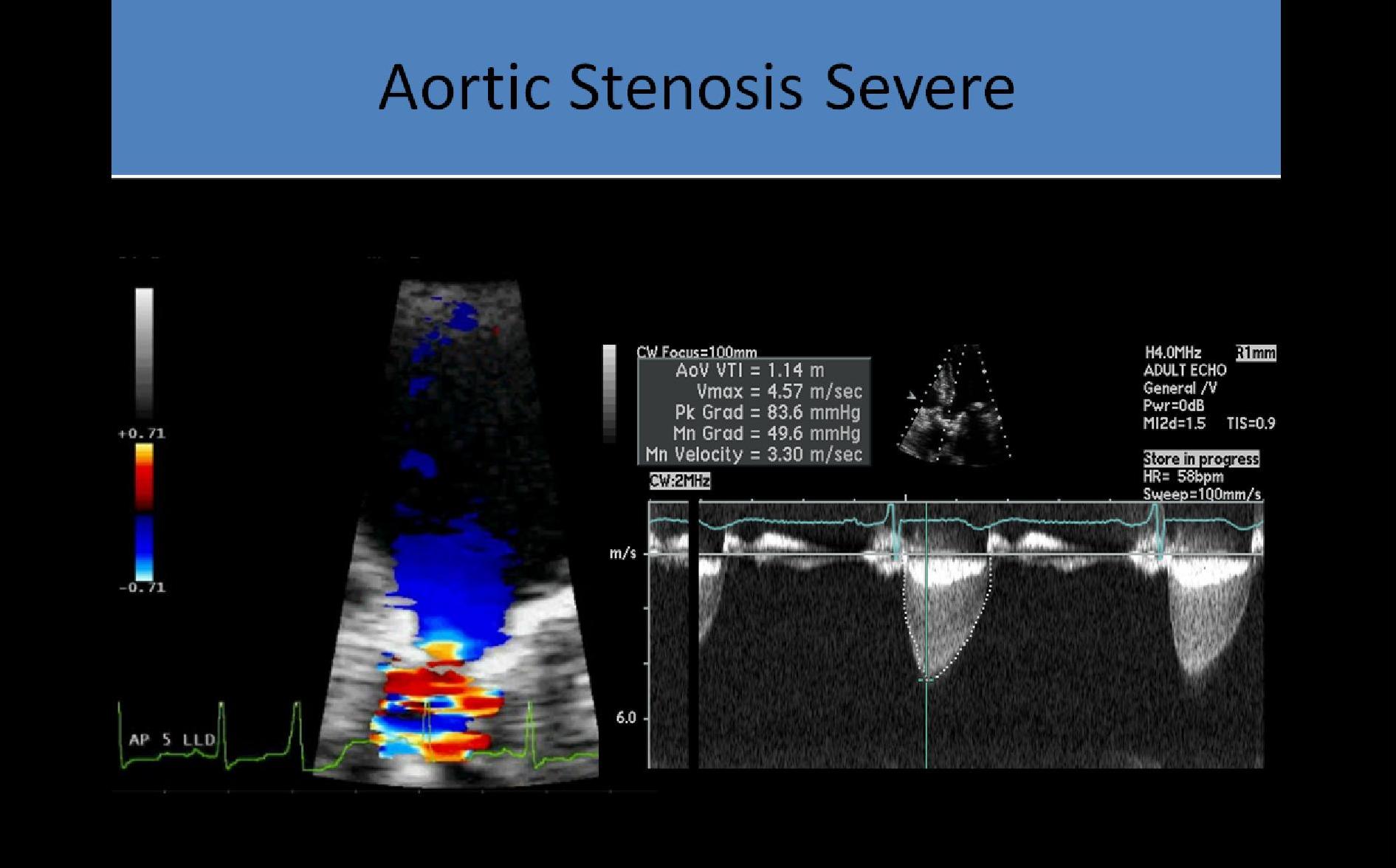
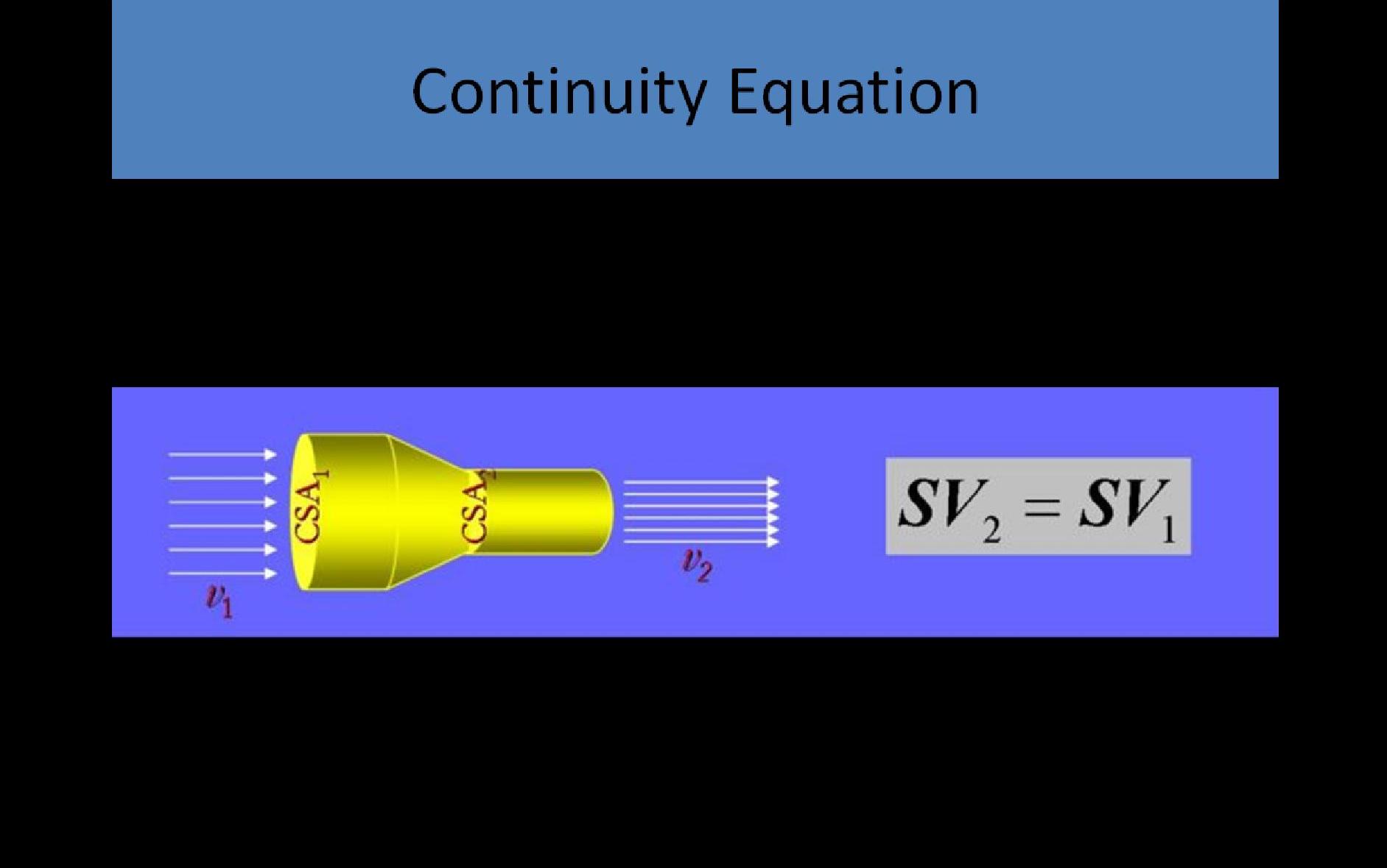
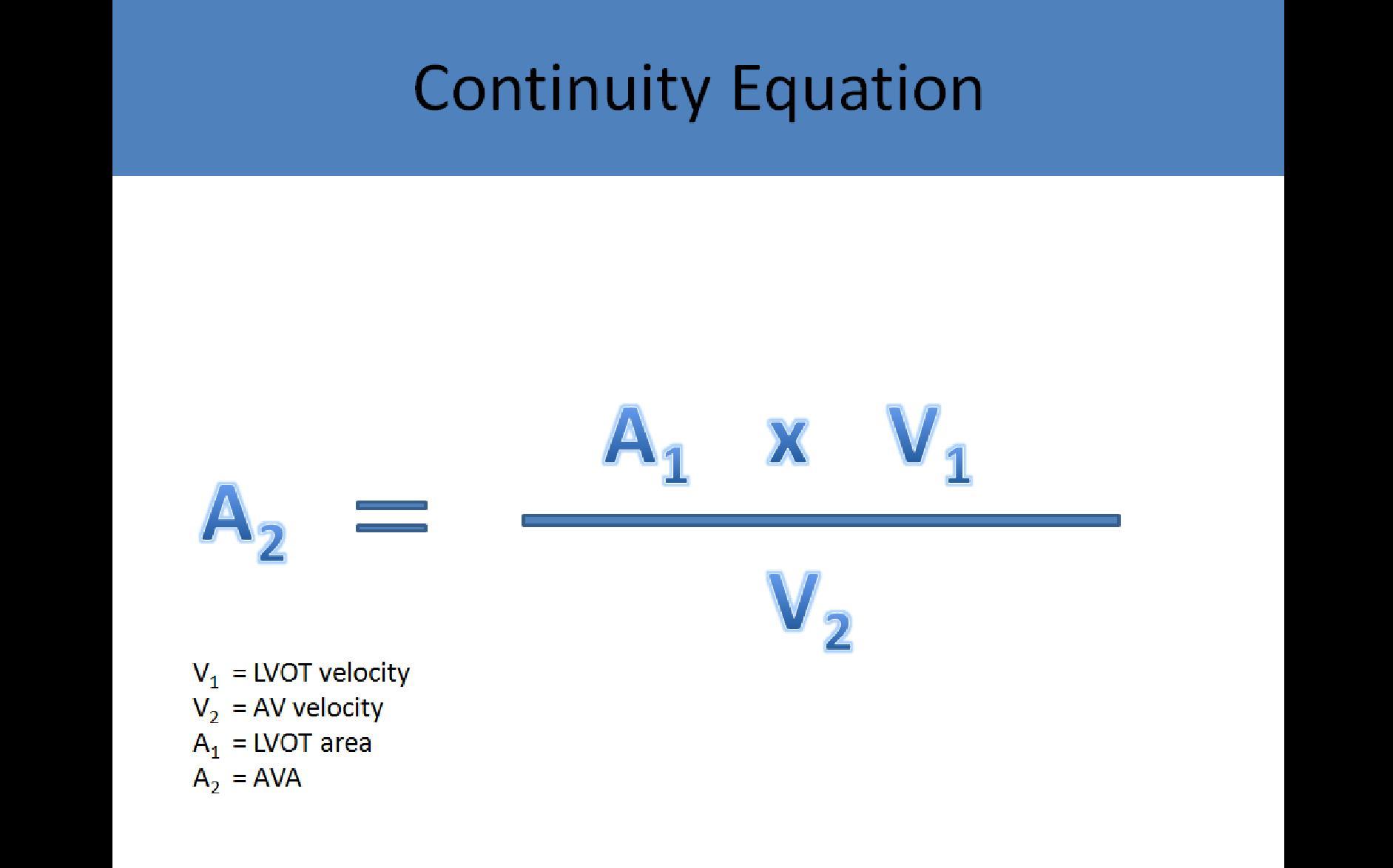
- Valve area calculated by continuity equation (independent of cardiac output, NOT affected by regurge):
> Mild: 1.5 – 2.0cm2
> Moderate: 1.0 - 1.5 cm2
> Severe: <1.0 cm2
- Dimensionless Orifice Index, VTI 1 / VTI 2 ratio (independent of cardiac output); Severe stenosis at <0.25
Peak Pressure Gradient (PPG):
- Mild (normal or increased cardiac output) <36 mmHg
- Moderate 37-64 mmHg
- Severe (normal or depressed cardiac output) >64 mmHg
- PPG is not an accurate method of assessing AS in patients with severe AI; LV becomes hypercontractile due to the continuous reprocessing of the same blood; PPG will be higher than the actual gradient related to the stenotic valve
Mean Pressure Gradient (MPG):
- Mild (normal or increased cardiac output) <20mmHg
- Moderate 21-40mmHg
- Severe (normal or depressed cardiac output) >40 mmHg
- Critical >50 mmHg
- MPG can be used to assess aortic stenosis in patients who also have aortic insufficiency
- MPG calculated on Doppler best correlates with the mean pressure gradient obtained during heart cath
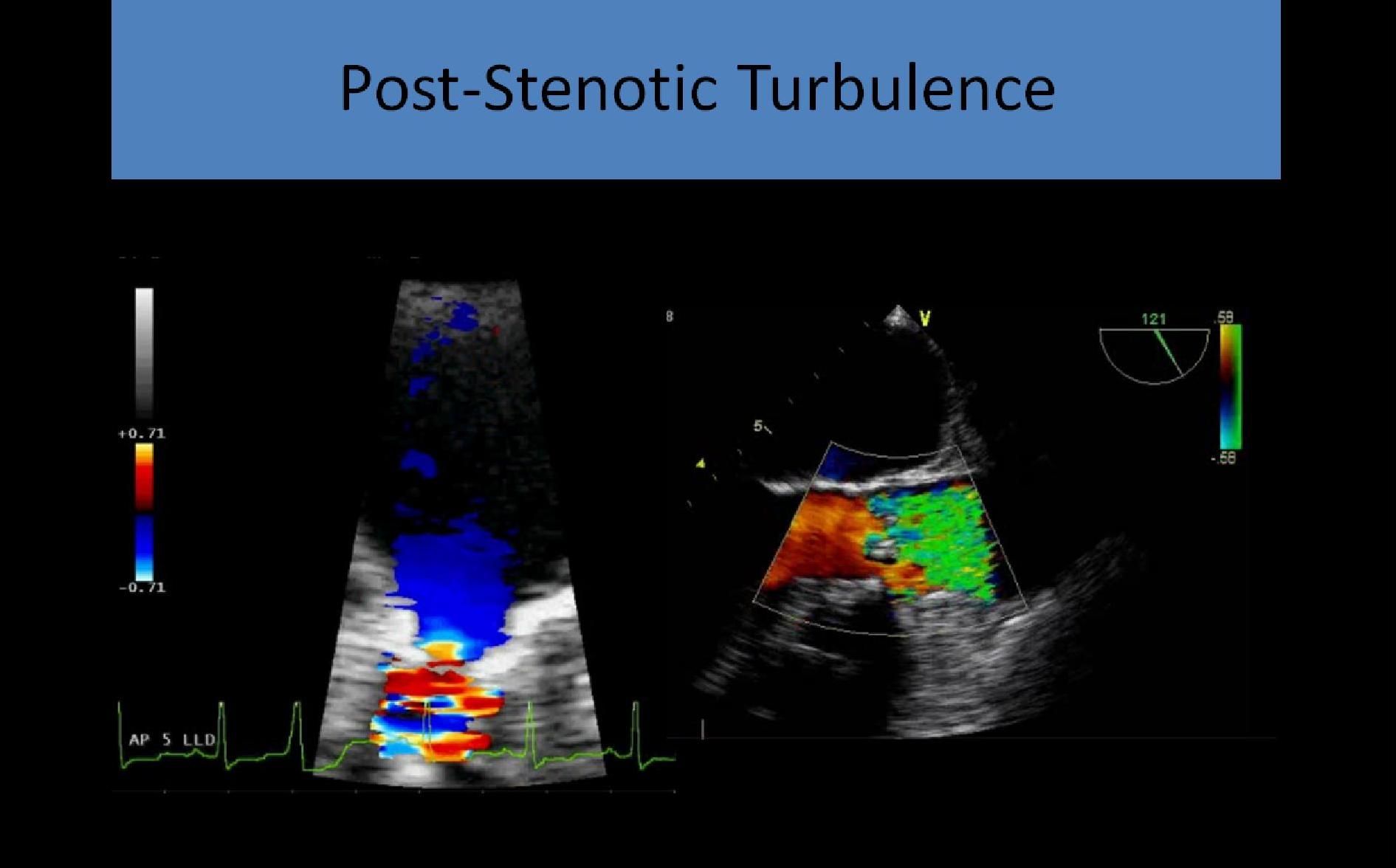
Associated Abnormalities:
- LVH with left heart pressure overload
- Dilated aortic root
- Turbulence distal to the valve
- Can be associated with CVA/Stroke due to decreased flow to brain and embolus potential from atherosclerotic disease on cusps
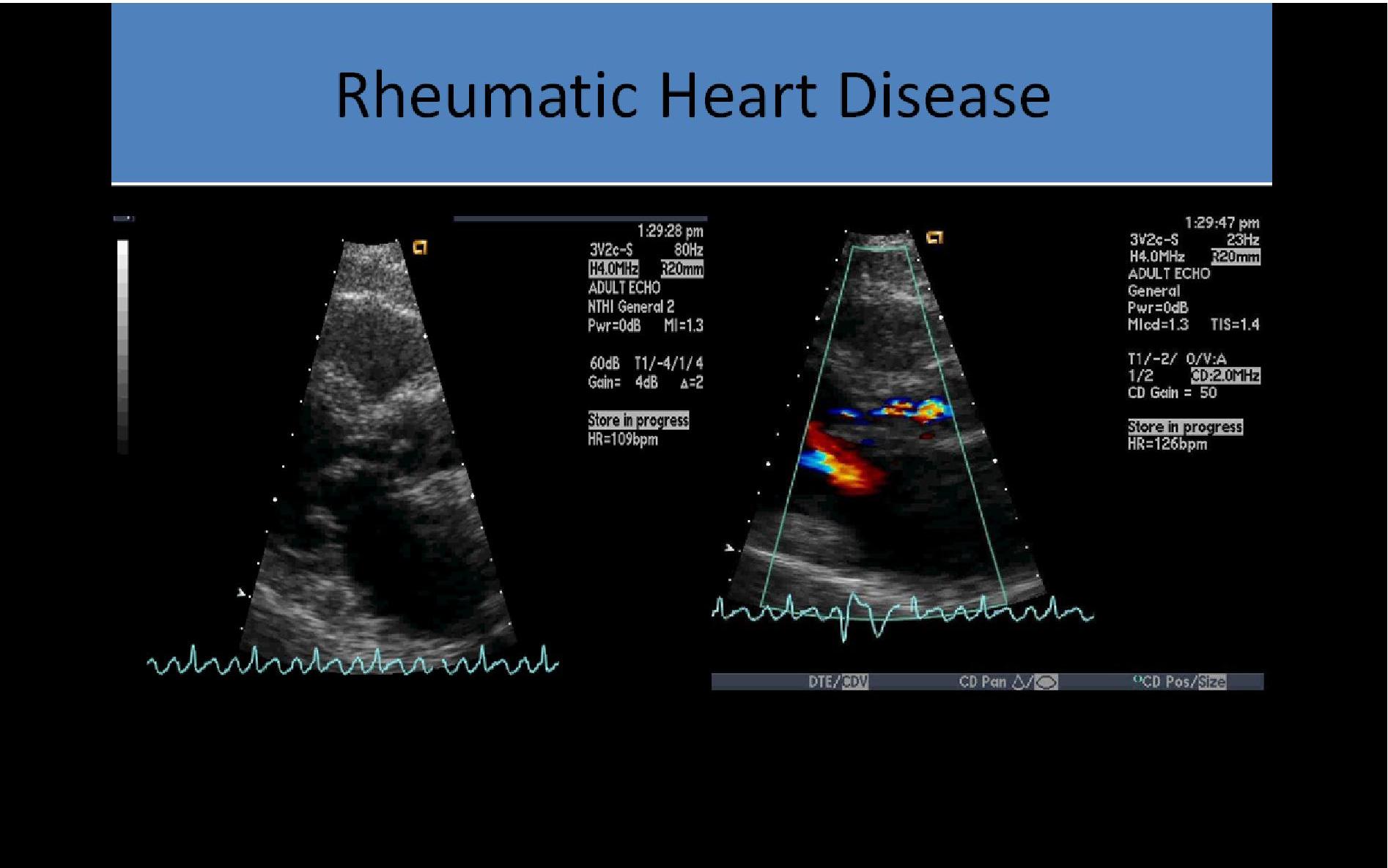
Rheumatic Heart Disease:
- Valvular degeneration and thickening from rheumatic heart disease usually affects BOTH the AV and MV where atherosclerotic disease usually affects one valve or the other
- May cause MS/MR and/or AS/AI
- Leads to same 2D/Doppler appearance as atherosclerotic stenosis
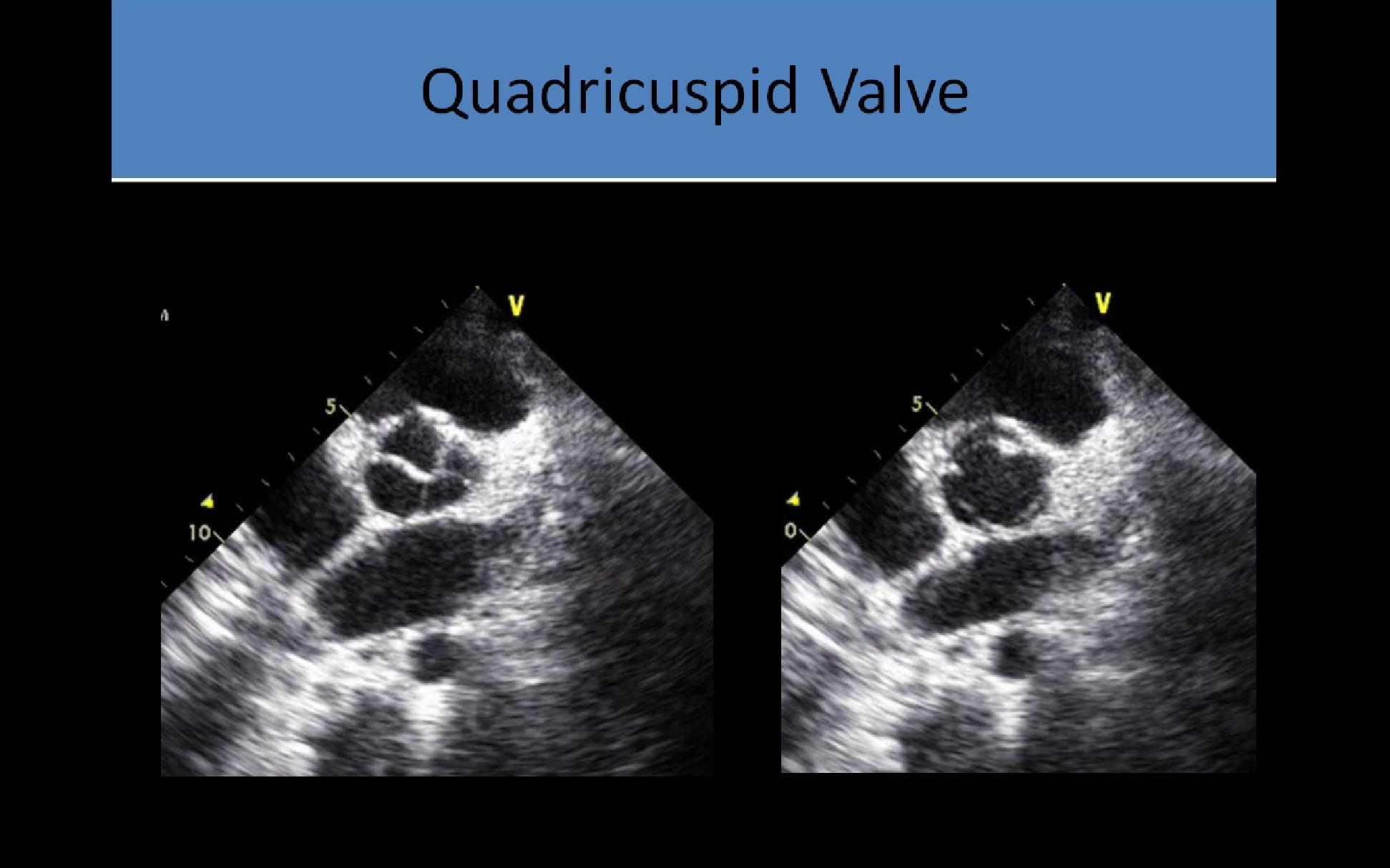
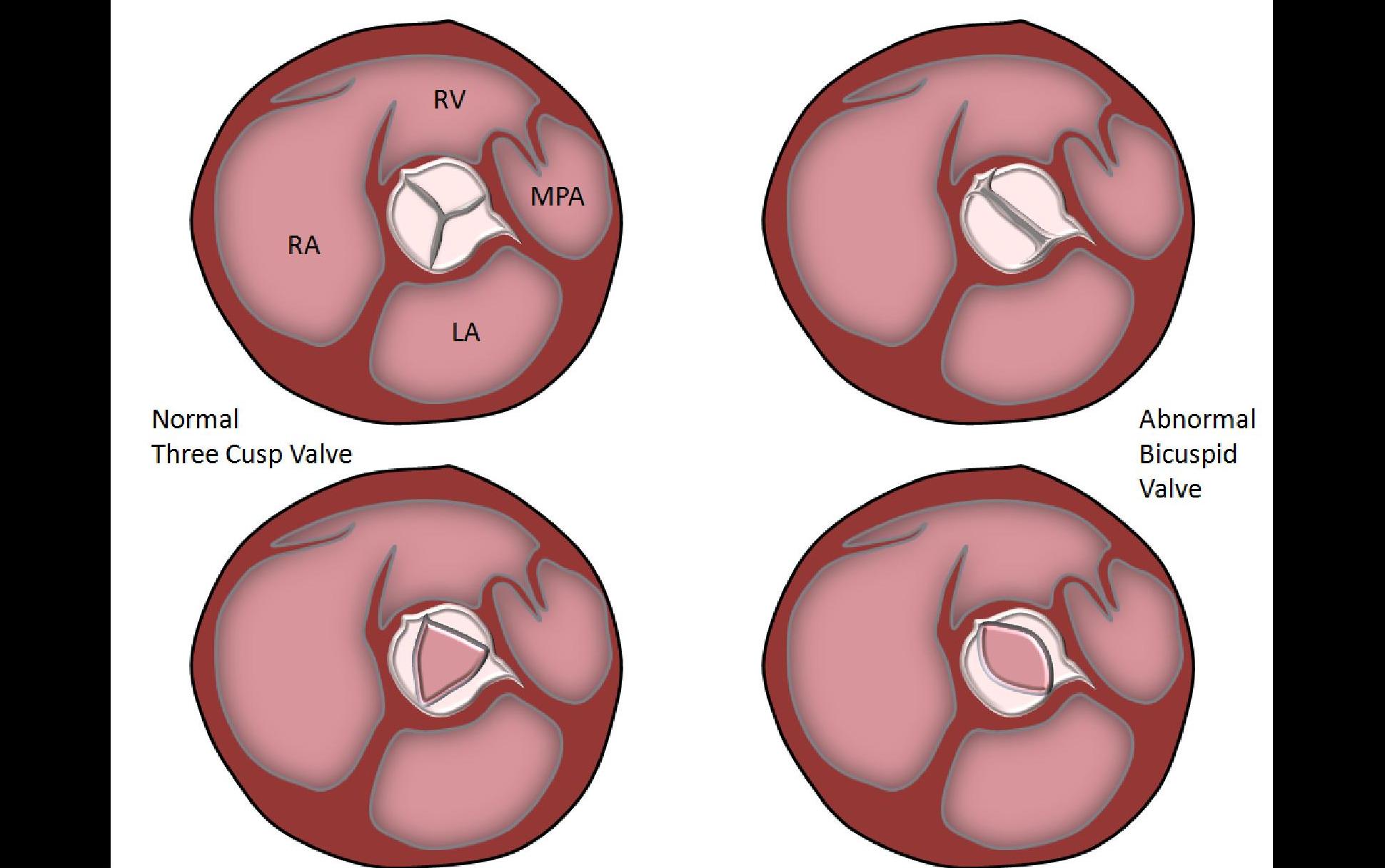
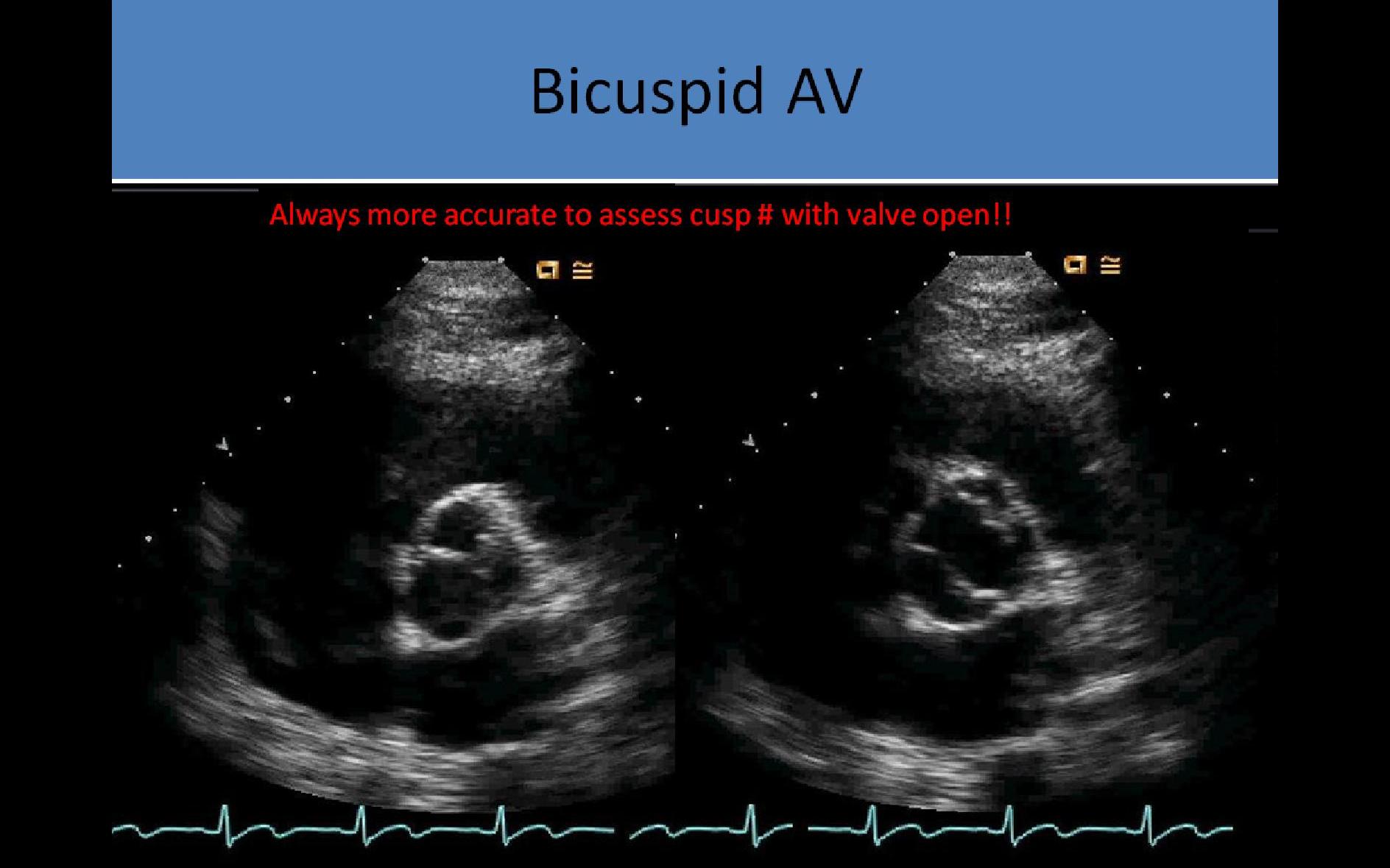
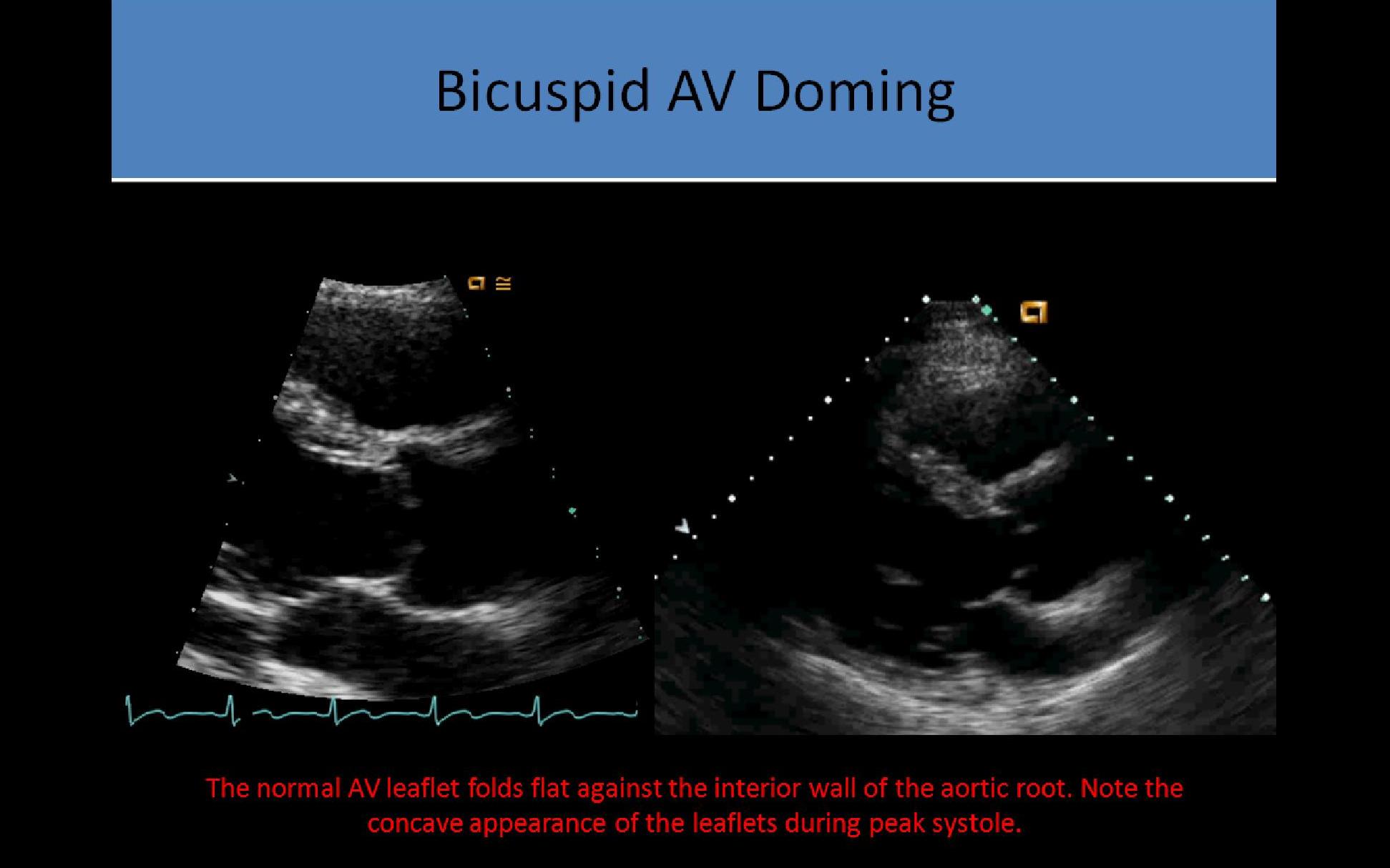
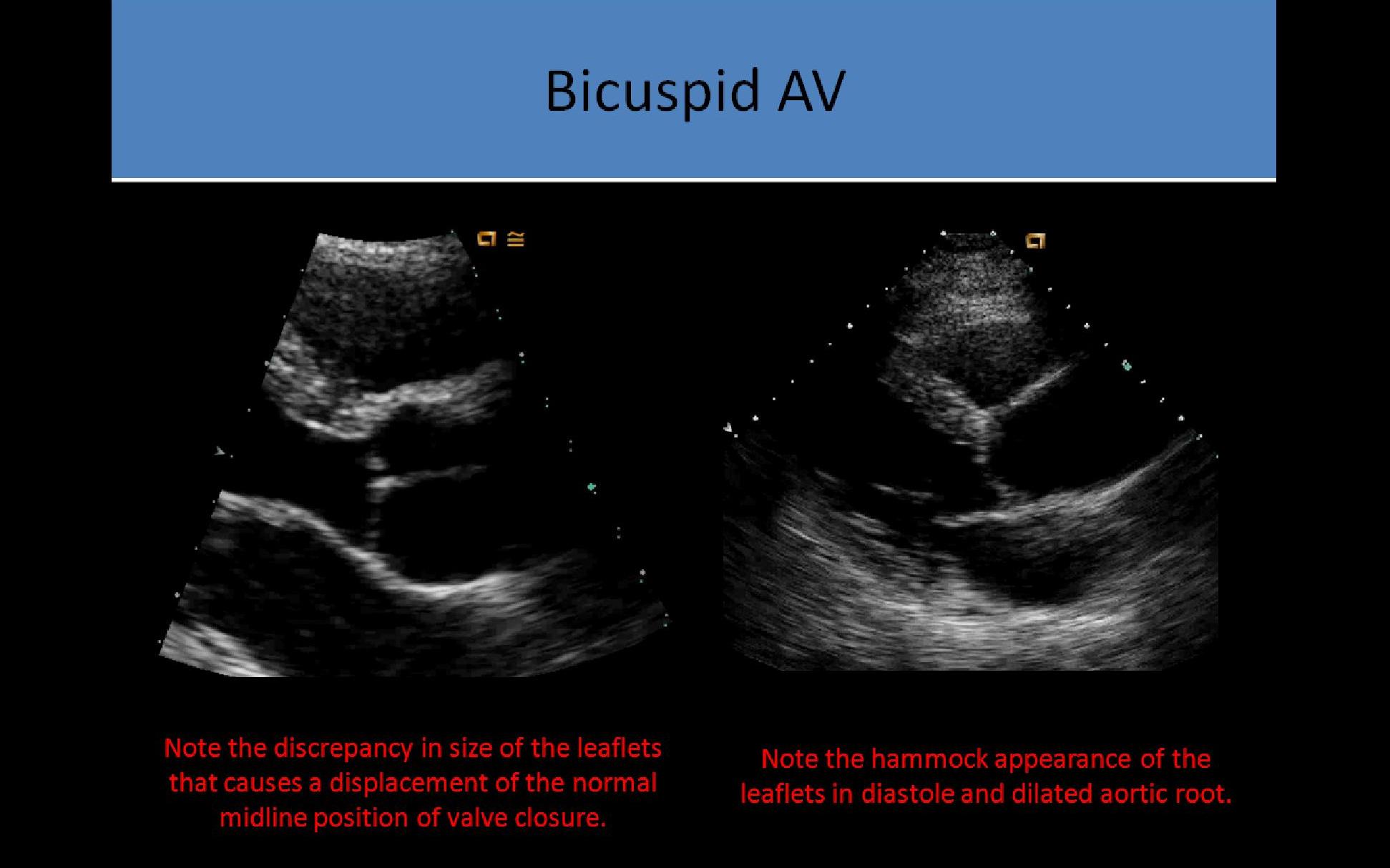
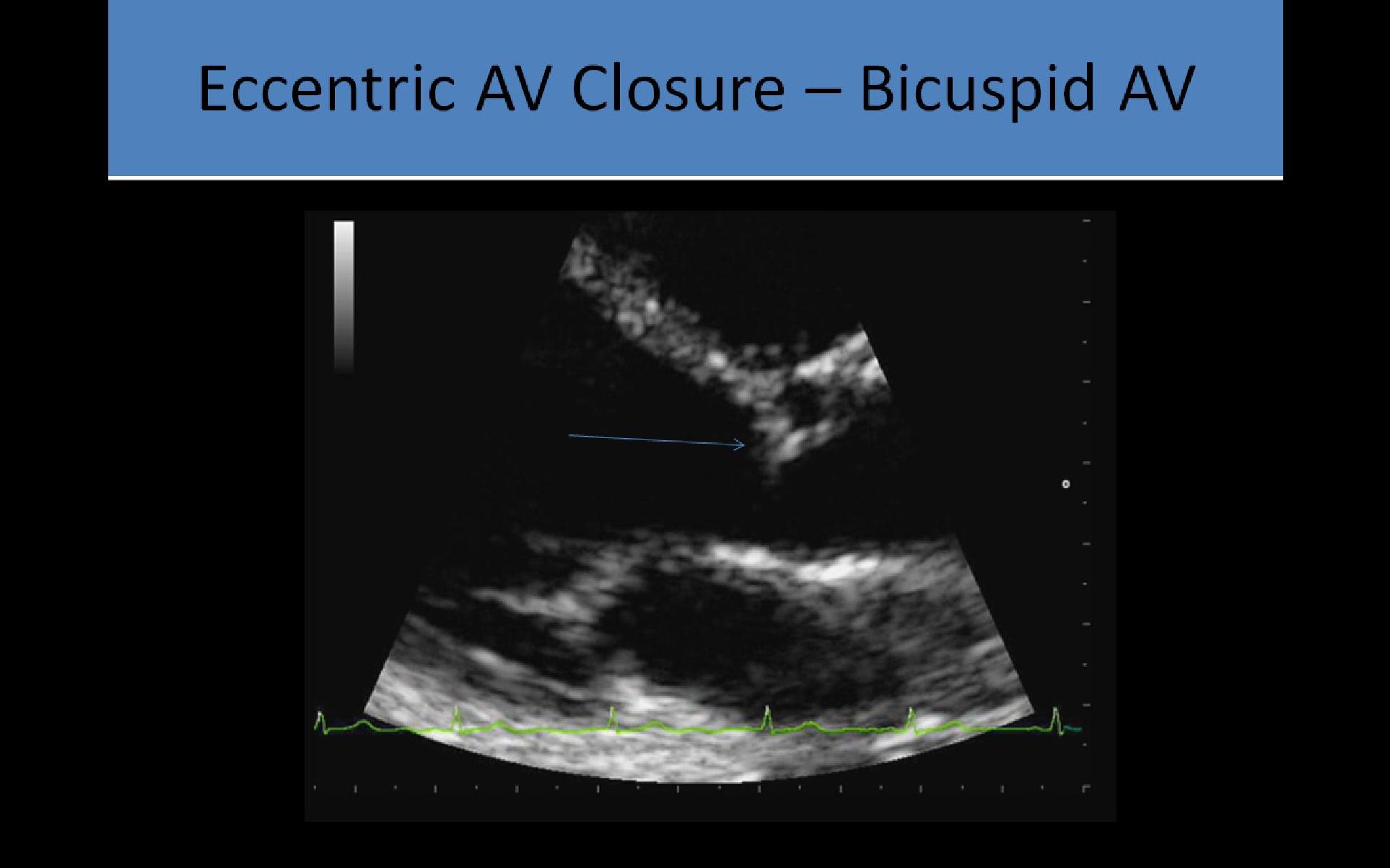
Congenital Aortic Valve Stenosis:
- Usually involves an abnormal leaflet number with restricted movement
- Can be unicuspid, bicuspid or quadricuspid
- Some bicuspid valves are composed of 3 leaflets with 2 fused together causing decreased AVA/stenosis
AV Regurgitation/Insufficiency:
Acute AV Regurgitation:
- Can be considered a critical finding with severe regurgitation
- Left ventricular pressure rises rapidly and can cause premature closure of the mitral valve and early opening of the aortic valve
- Left ventricle dimension is usually NORMAL with the acute onset of the regurgitation
- Restrictive filling pattern demonstrated by E/A > 1.5 and short deceleration time
Symptoms:
- Chest pain
- Orthopnea - difficulty breathing when supine
- Cough
Common Causes:
- Infective endocarditis
- Aortic dissection of the ascending aorta
- Trauma
Symptoms:
- Heart Failure
- Chest Pain
- Fatigue
- Dyspnea/Orthopnea
- High pitched, early diastolic decrescendo murmur heard along the left sternal border; severity of the murmur is inversely proportional to the duration of the regurgitation
- Austin Flint murmur - severe AI; low frequency diastolic murmur
Common Causes:
- Inadequate leaflet coaptation
- Ruptured leaflet or vegetation
- Dilatation of the valve annulus
- Bacterial endocarditis
- Fibrosis/Calcification of the leaflets
- Rheumatic heart disease
- Chronic volume overload of the left ventricle may cause dilatation
- Aortic valve is more resistent to regurgitation than the mitral valve due to structural differences in the valve
- Aortic valve is the most resistent to regurgitation when compared to all of the heart valves
Treatment:
- Valve replacement indicated when the left ventricle is significantly enlarged and fractional shortening of the ventricle is reduced
- End diastolic dimension >5.5cm and FS% <25%
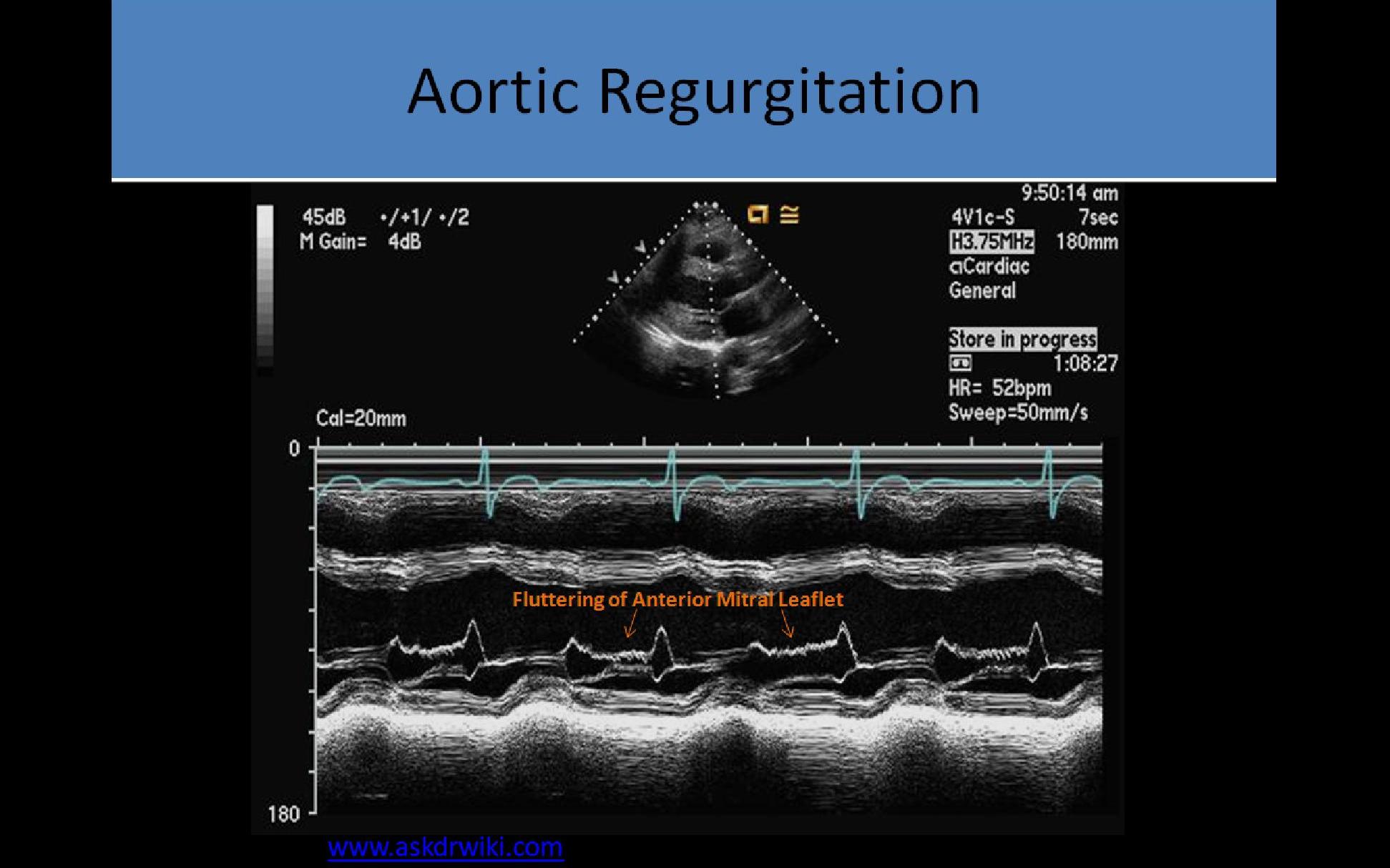
2D/M-Mode:
- Flow starts before the mitral valve opens and continues until shortly after it closes
- Best recorded with a transducer in apical position or from a suprasternal location
- Fluttering of the anterior leaflet of MV or IVS in diastole
- May see premature closure of the MV and reverse doming of the MV in diastole
- Chronic AI leads to LV volume overload and hypercontractile LV motion
- LA dilatation occurs with significant chronic aortic insufficiency
- Significant AI can cause early closure of the MV in diastole due to increased diastolic pressures in the LV
- Mild: Little to no effect
- Moderate/Severe: LV dilatation and hypercontractility, mild LA enlargement
- Early MV closure seen on m-mode with severe AI
- May cause IVS fluttering and anterior MV leaflet vibration in diastole due to eccentric jet
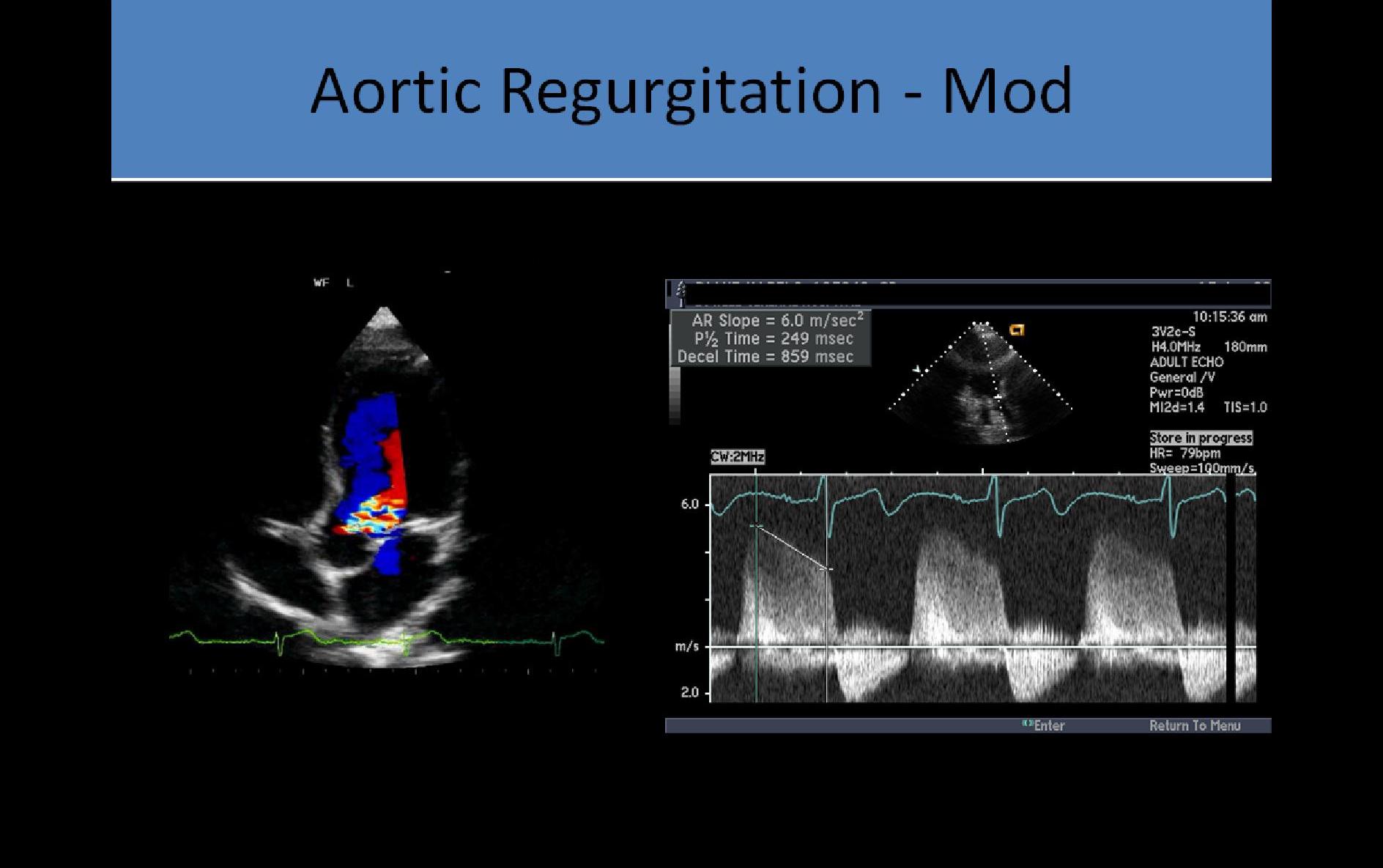
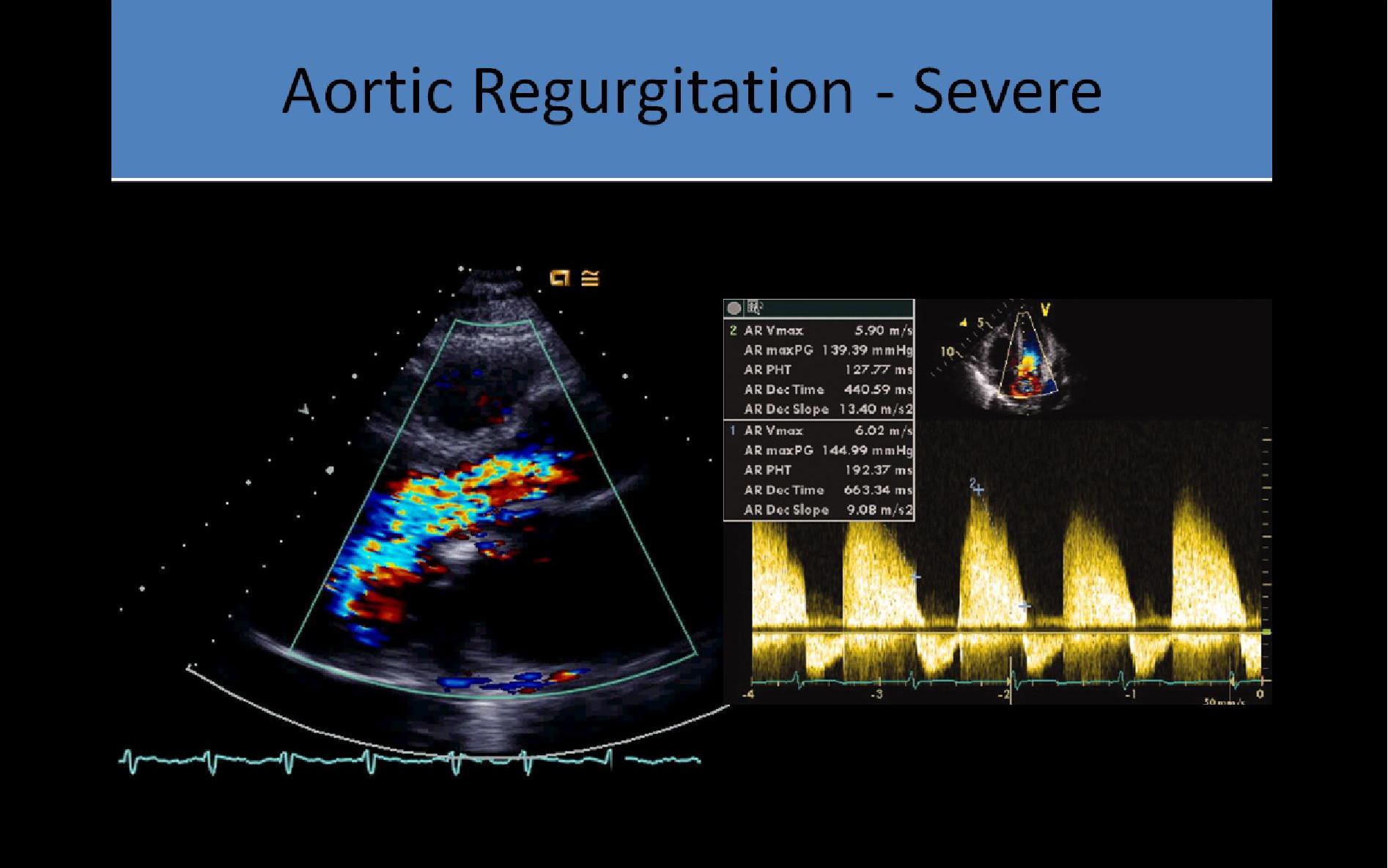
Color Doppler:
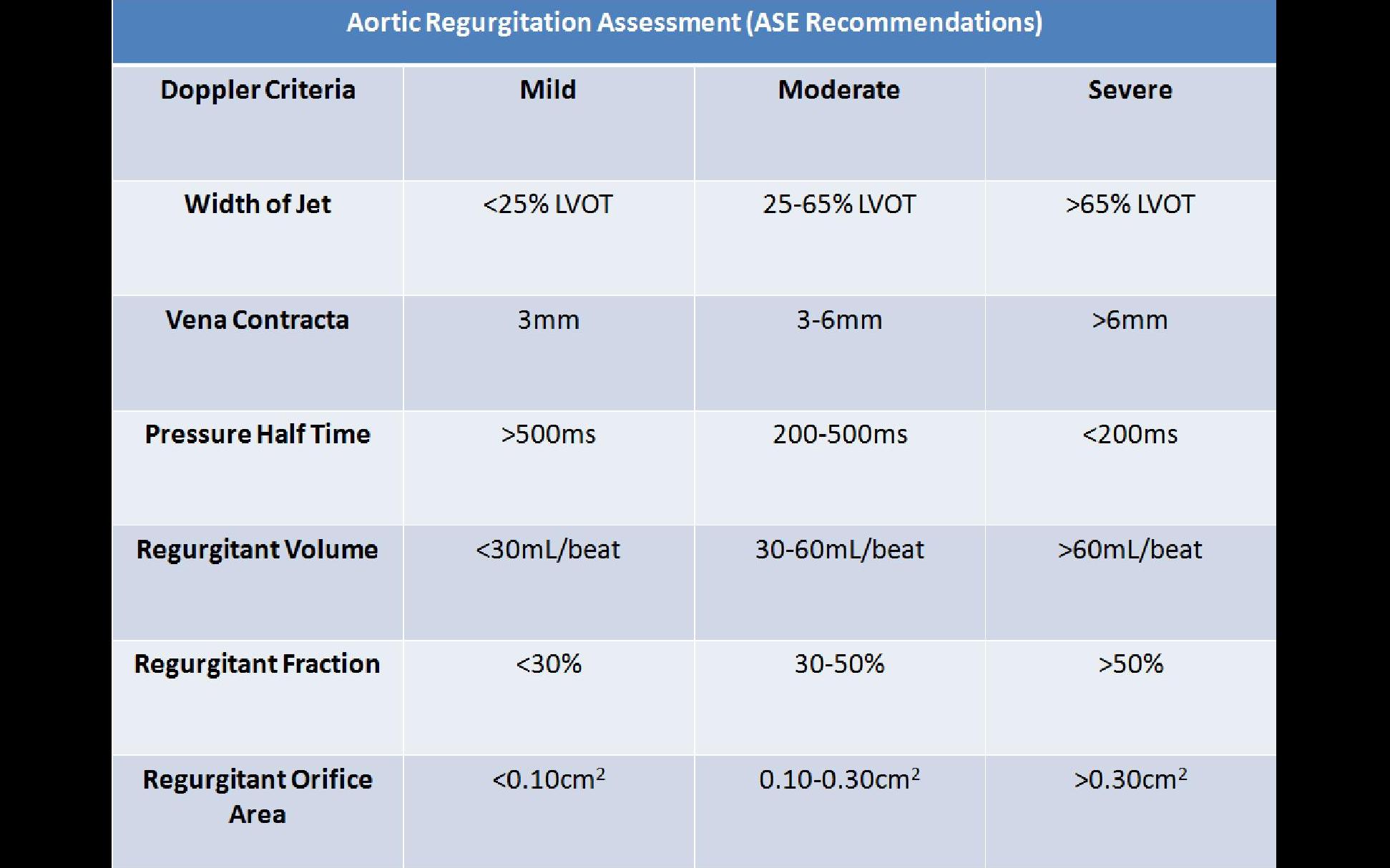
If the regurgitation jet fills LVOT at a ratio:
- <30% suggests mild regurgitation
- 30% to 60% suggests moderate regurgitation
- >60% suggests severe regurgitation
- Vena contracta <0.3cm is mild; >0.6cm is severe
- Vena contracta width can be performed at the narrowest segment of the regurgitant jet between proximal flow convergence and distal jet expansion
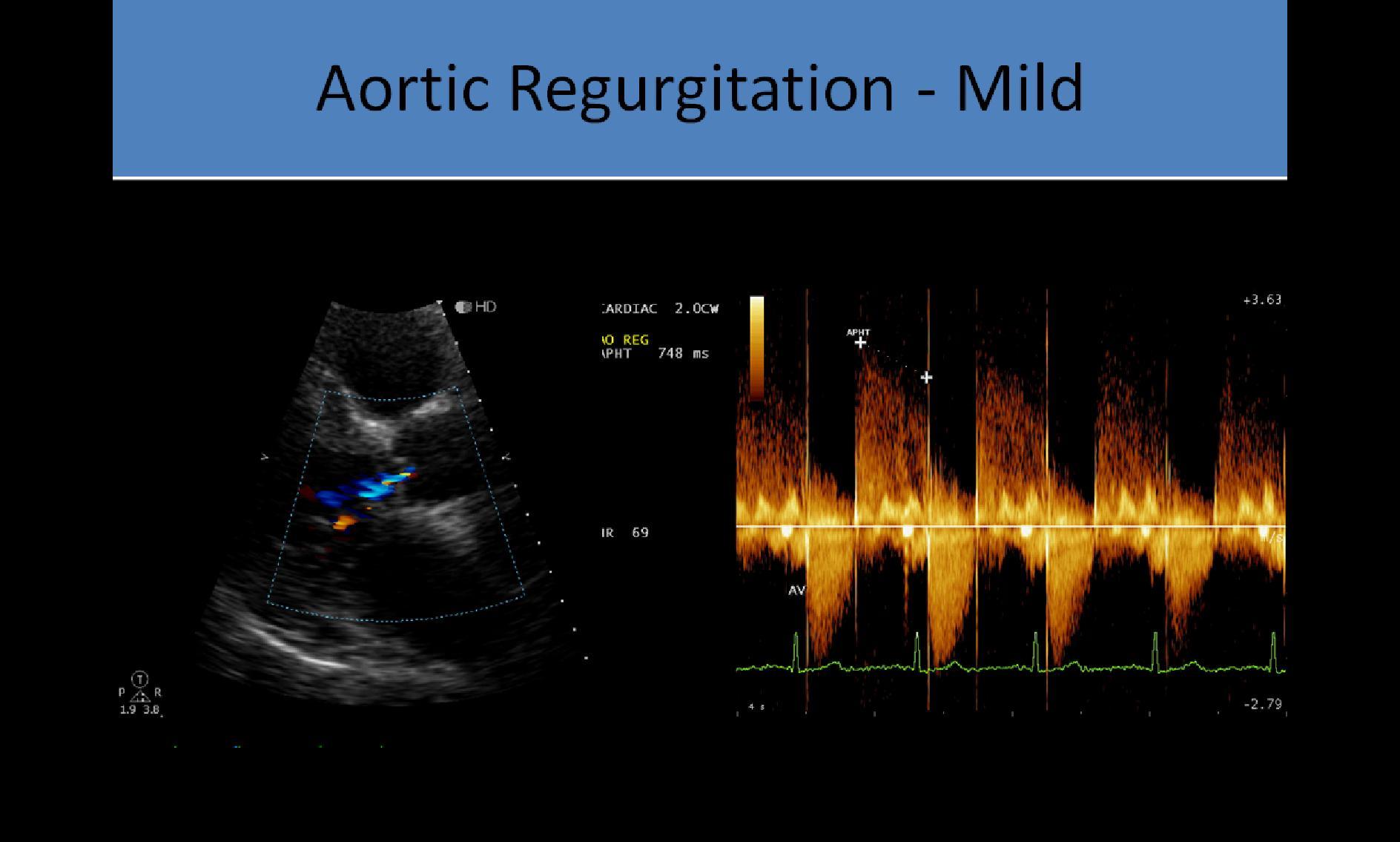
PW/CW Doppler:
- The denser the jet appearance on the Doppler display, the more severe the regurgitation
- Peak velocity of the regurgitation indicates the maximum pressure gradient between the aorta and the LV in diastole, not helpful in diagnosing severity of the regurgitation; 70mmHg = about 4m/s peak velocity in the normal heart
- Pressure half-time of the slope of the Doppler tracing used to assess severity of regurgitation
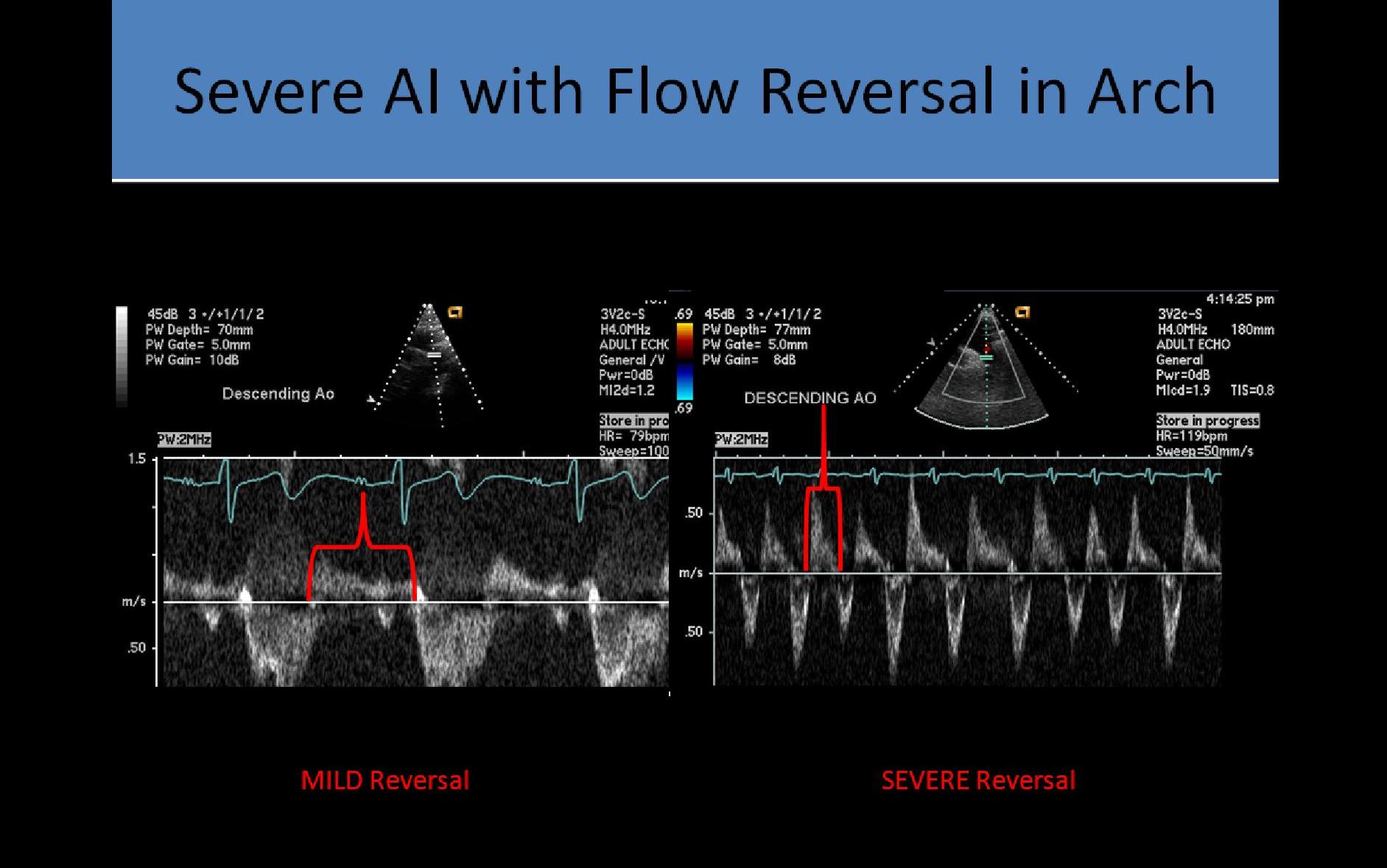
- SSN notch used to assess flow reversal in the descending aorta
- Pressure half-time: time it takes for the pressure gradient to reduce by 1/2
> shorter time = more severe AI
> Mild >500 msec
> Moderate 200-500 msec
> Severe <200 msec
- Moderate : early diastolic flow reversal in descending aorta
- Severe: flow reversal throughout diastole in the descending aorta; causes overestimation of the peak pressure gradient through a stenotic AV due to the hypercontractile motion of the LV
- The waveform of mitral stenosis and aortic regurgitation can be difficult to distinguish on the Doppler tracing; if the flow pattern begins before the mitral valve opens, the waveform is from aortic regurgitation
Aortic Fenestration:
- Hole or "window-like" opening in the leaflet or between the leaflets
- Can be congenital or acquired
- Causes aortic regurgitation
- Associated with increased risk of valve rupture
- M-mode used to diagnose; diastolic flutter of the AV leaflets considered a definitive finding
- TTE Color and Doppler evaluation cannot distinguish the fenestration as the cause of the leak
- TEE can be used to confirm the m-mode diagnosis
- Can be a complication of a heart cath, if the catheter punctures the valve apparatus
