
.jpg)
Abdominal Aorta: Sonographic Evaluation and Disease
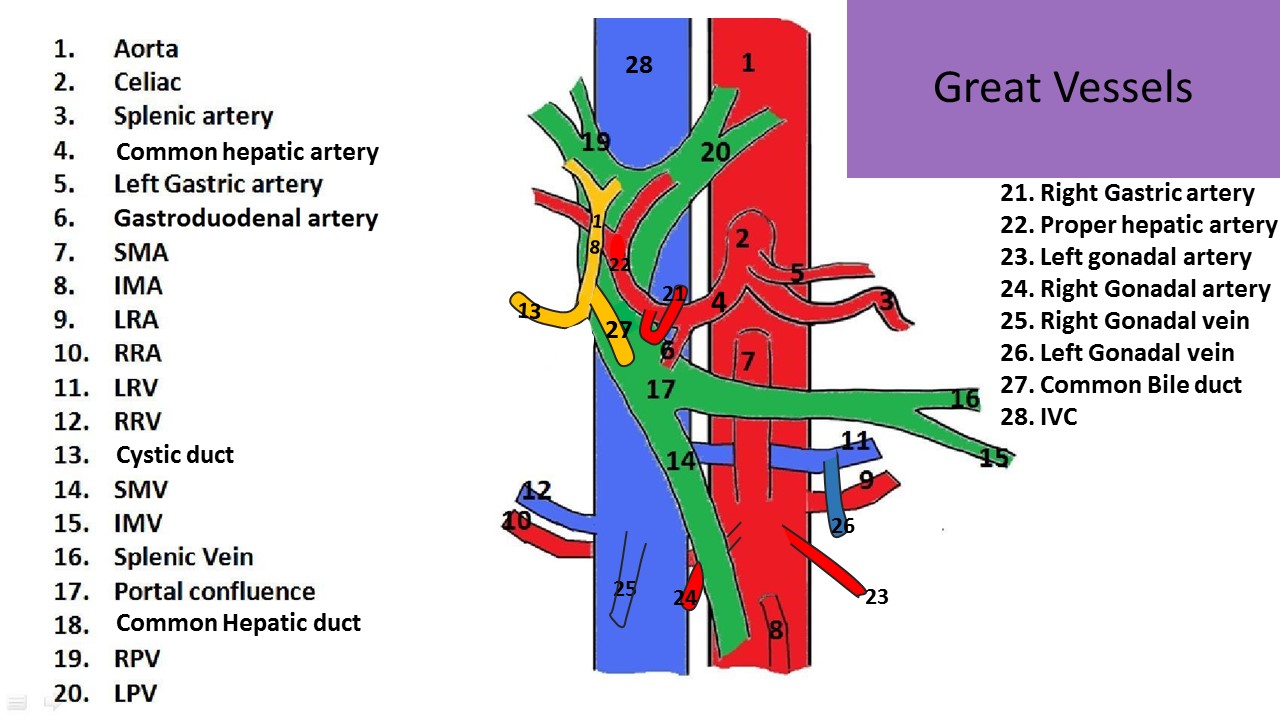
Blood Vessel Anatomy:
- Tunica Intima-inner layer endothelial cells, basement membrane is the innermost layer of intimal cells
- Tunica Media-middle layer, muscle, thicker and more organized layer in arteries than veins
- Tunica Adventitia/Externa-Outer Layer, epithelial cells
***Veins have thinner media layer to allow flexibility of lumen size with varied flow volume***
AORTA
Anatomy:
- Trunk artery
- Arises from left ventricle
- Courses inferior through chest and enters the abdomen through the diaphragm
- Located anterior and to the left of the spine and to the left of the IVC
- Most posterior abdominal vessel
- More posterior than the IVC until the umbilicus level where it lies more anterior than the IVC
- Distributes oxygenated blood to organs and limbs
- In most cases branches of the aorta are named after the organs they are feeding
Paired Branches:
- Suprarenal arteries - supply adrenal glands
- Renal arteries - supply kidneys
- Gonadal arteries - supply ovaries/testicles
- Lumbar arteries
- Common iliac arteries
Unpaired Branches:
- Celiac Axis - 1st abdominal branch of aorta, supplies blood to common hepatic artery, splenic artery and left gastric artery
- Superior Mesenteric Artery(SMA)
- Inferior Mesenteric Artery (IMA)
- Median Sacral Artery
Anterior Branches: from superior to inferior
- Celiac Axis
- Superior Mesenteric Artery(SMA)
- Inferior Mesenteric Artery (IMA)
- Gonadal Arteries
- Median Sacral Artery
Lateral Branches: from superior to inferior
- Suprarenal Arteries
- Renal Arteries
- Common Iliac Arteries
COMMON ILIAC ARTERIES:
- Bifurcation at L3-4 vertebra, umbilicus level
- Supplies legs and pelvis
- High resistance flow
- Above the umbilicus, abdominal arteries are posterior to veins
- Below the umbilicus, the abdominal/pelvic arteries are anterior to the veins
- Evaluated for arterial pathology in longitudinal and transverse planes

Indications to Scan the Aorta:
- Abdominal pain
- Pulsatile mass
- Aneurysm seen on x-ray
- F/U aneurysm
- Trauma
Lab Testing:
- Hematocrit - decreased levels can indicate an active bleed in the body
- Low hematocrit could be due to an aneurysm that is leaking into the abdomen
Exam Technique:
- 2.5MHz to 6.5MHz adult probe
- 4MHz to 8MHz pediatric probe
- Patient must be NPO 8-12hrs prior to the exam to best visualize the abdominal vasculature
- Multiple patient positions can help view the aorta behind gas containing bowel loops
- Supine, oblique and decubitus positions may all be necessary for optimal evaluation
- A transverse view can demonstrate a transverse image of both great vessels on the same image
- To obtain a longitudinal view of the aorta and IVC on the same image:
- Position the patient in a decubitus position
- Use a coronal approach to angle through the abdomen to visualize the aorta and IVC simultaneously
- A right coronal approach will demonstrate the aorta as the posterior vessel on the image
- A left coronal approach will demonstrate the IVC as the posterior vessel on the image
- Right posterior oblique position can be especially helpful for evaluating the distal aorta bifurcation into the common iliac arteries
- Identifying the celiac axis guarantees a complete evaluation of the proximal segment
- Identifying the aortic bifurcation guarantees a complete evaluation of the infrarenal segment
- 2D, Color and Doppler evaluation of proximal, mid and distal segments with iliac arteries
Sonographic Appearance:
- Best anatomic landmark in abdomen
- Longitudinal - hollow tube anterior to spine
- Transverse - circular structure to the left of the comma shaped IVC
- Gradual tapering as it courses distally
- Becomes more anterior in the abdomen as it courses distally
Average Normal Measurements:
Proximal 2.0-2.6 cm
Mid 1.6-2.4 cm
Distal 1.1-2.0 cm
Iliacs 0.6-1.4 cm
- AP Dimensions are obtained in longitudinal plane, from outer wall to outer wall of the vessel
- Width Dimensions are obtained in the transverse plane, from outer wall to outer wall of the vessel
Doppler of the Aorta:
- High resistance
- Clean spectral window
- Biphasic above renal arteries due to low resistance branches to organs
- Triphasic below renal arteries; supplies lower extremities which cause an increase in resistance
- Occlusive disease may change resistance and pulsatility of waveform
- Aneurysmal disease may show increased turbulence, especially with color Doppler







PATHOLOGY
Aortic Ectasia:
- Lack of tapering of the aorta as it travels distally, size remains constant from proximal to distal portions
- Can be a precursor to aneurysm formation
Abdominal Aortic Aneurysm:
- Focal dilatation of the aorta >3cm or increase in diameter >50% between two adjacent segments
- Most commonly caused by atherosclerotic disease
- All three layers of the arterial wall are stretched
- Risk factors include male gender, family history, smoking, chronic HTN
- Anemia and low hematocrit levels can be an indicator for a slow bleed from an aneurysm
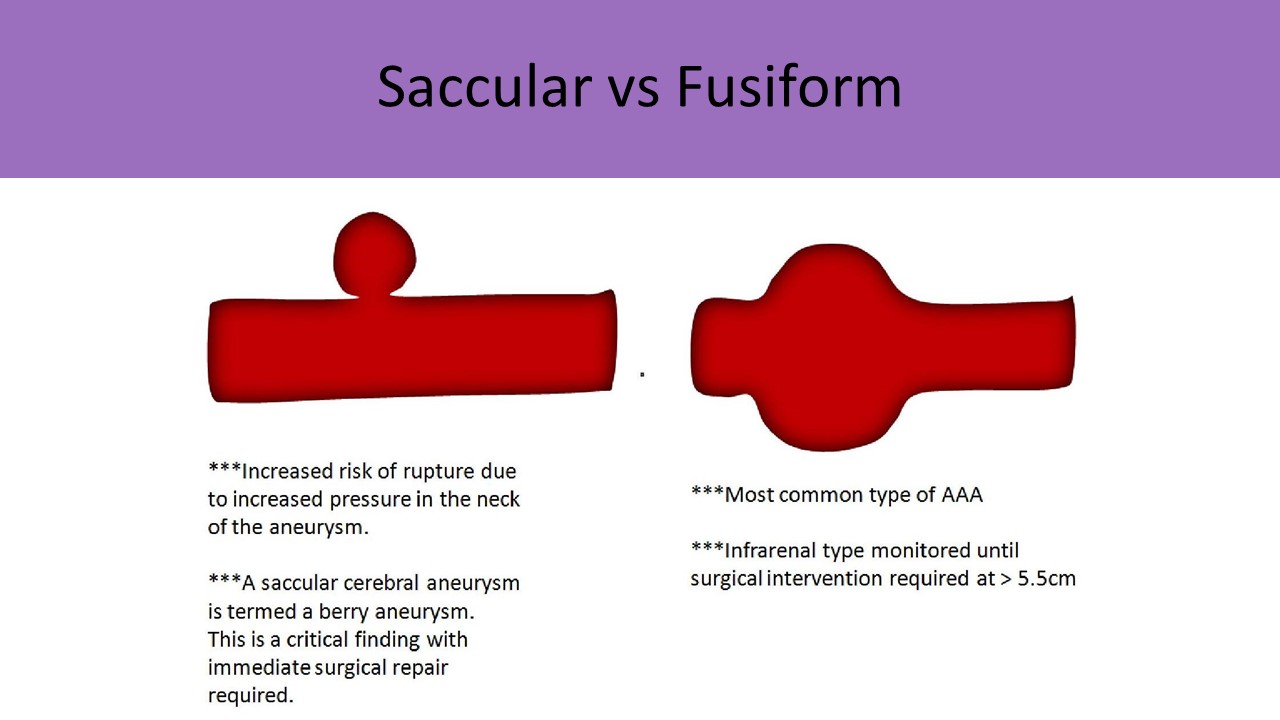
- Types:
- Saccular - localized round outpouching, may have small stalk
- Fusiform - vessel wall stretches in a circumferential manner; most common type
- Berry - tiny out pouching, usually found in the cerebrum and splanchnic arteries
- Mycotic - infected aneurysm; seen with syphilis
- Above the Renal Arteries - immediate surgical intervention
- Below the Renal Arteries - Most common location of fusiform aneurysms
- Surgical intervention at a diameter >5.5cm
- Iliac, common femoral and popliteal arteries can have associated aneurysm formation
- Common iliac artery diameter >1.5 cm indicates aneurysm formation
- If AAA identified, measure the diameters of the common femoral and popliteal arteries
- CFA and popliteal artery aneurysms are defined as a >50% increase in diameter compared to adjacent segment
- Requires follow up exams after AAA is first identified
- Annual follow up on AAA 4-4.4cm diameter
- Semiannual follow up on AAA >4.5cm
Complications:
- Rupture - blood collects in the perirenal space first
- Decreased flow to lower extremities
- Blue Toe Syndrome with thrombus accumulation and embolization
- Affects renal circulation and systemic blood pressure, if suprarenal or juxtarenal in location
- Large AAA can compress IVC causing reduced flow toward the heart and pedal edema
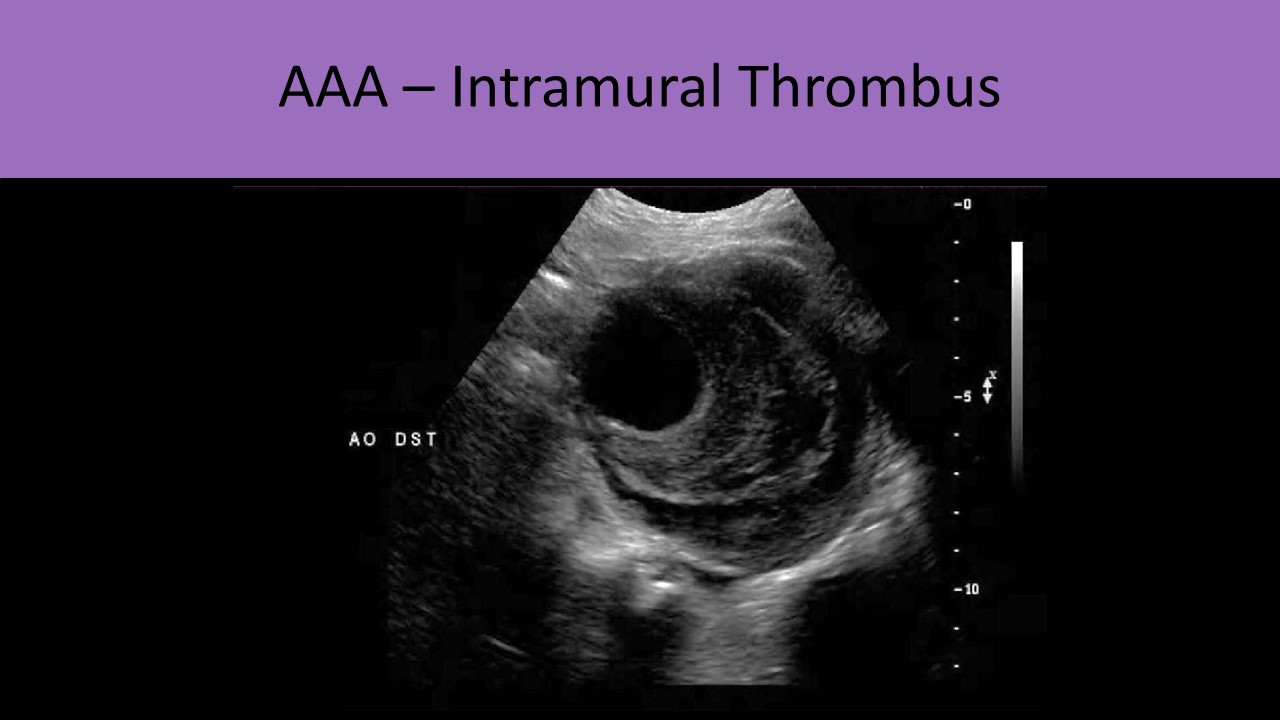
Sonographic Appearance:
- Identifying the celiac axis guarantees a complete evaluation of the proximal segment
- Identifying the aortic bifurcation guarantees a complete evaluation of the infrarenal segment
- Goal of the exam is to find the location of the maximum diameter of the aorta
- The greatest diameter of the abdominal aortic segment should be at the level of the celiac axis
- Longitudinal images provide the best view for accurate measurements perpendicular to the axis of the vessel
- Measure true vessel size from outer edge of the wall to outer edge of the wall
- Enlarged vessel >3cm or >50% increase in diameter compared to adjacent segment
- Possible thrombus accumulation causes echogenic debris levels within the lumen
- Measure true lumen size, if thrombus accumulation present
- Measure the length of the affected segment
- Document AAA location related to renal arteries
- Turbulence seen with Color and PW Doppler evaluation
- Yin Yang Sign - describes the swirling blood in the body of the aneurysm




Aneurysms of the Splanchnic Arteries:
- Splenic Artery
- Most common splanchnic artery aneurysm
- Associated with pancreatic inflammation, peptic ulcers, patients with more than 2 pregnancies (multigravida) and trauma
- Usually multiple
- More common in women
- May cause bruit in LUQ
- Critical finding due to rupture risk
- Hepatic Artery
- 2nd most common type
- Most are in the extrahepatic segment
- Associated with systemic infection and trauma
- SMA
- Least common type
- Associated with cystic medial necrosis
- Percutaneous stent or graft placement through the groin is the standard treatment for infrarenal aortic aneurysms
- The grafts must be monitored by serial ultrasound exams to assess for endoleak
- 3-6 month serial exams in first year, 6-12 months after the first year
- Normally the native aortic sac will decrease in size over time
- If a leak is present, the native sac will increase in size between exams
- The native aortic sac should be measured in the transverse plane
- If the aortic sac expands more than 0.6cm between exams, a leak should be suspected
- Color Doppler can be helpful in identifying blood flowing out of the graft into the native sac
- Four Types of Leaks
- Type I: leak at the graft attachment site
- Type II: retrograde flow into the native sac from the lumbar artery or IMA
- Type III: defect in the graft
- Type IV: graft material too porous and allowing blood through the fabric mesh



Blue Toe Syndrome:
- Embolic material lodges in digital arteries in toes leading to cyanosis of the distal tissues
- Causes: Thrombus in an aortic aneurysm, arteritis, ulcerated atherosclerotic lesions, some angiography procedures
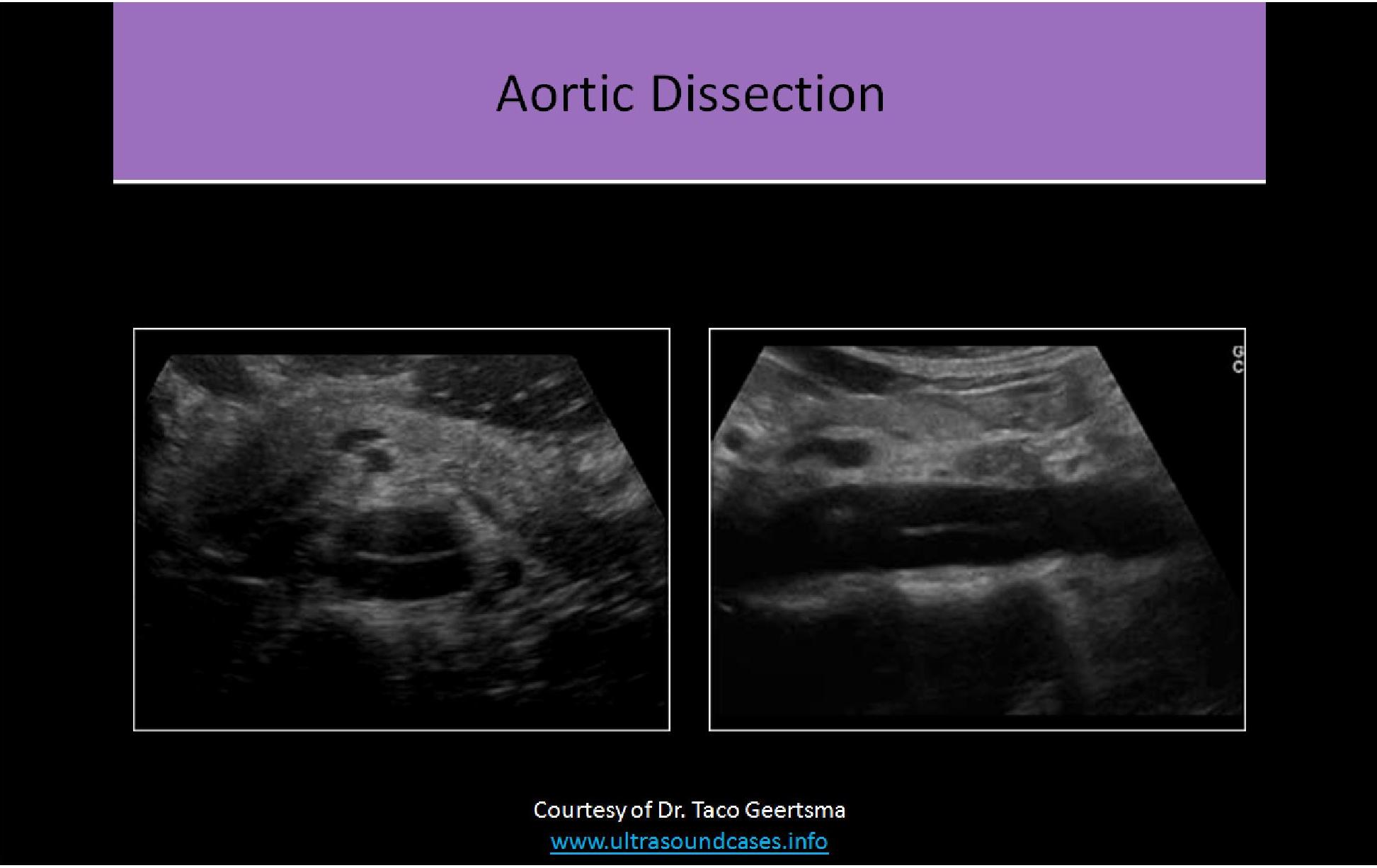
Dissection:
- Intimal layer tears and allows flow between the intima and media layers into a blind pocket (false lumen)
- Remaining lumen (true lumen) is decreased in size due to flap with blood flow beneath it
- Causes weakened vessel wall, risk of vessel rupture
- Thrombosis can occur in the false lumen which can cause a significant stenosis/occlusion in the vessel and ischemia distal to the dissection
- Most commonly occurs in the aortic arch due to the shearing forces of the blood as it rounds the curve of the arch
- Surgical intervention required immediately due to significant risk of rupture
- Debakey Classification:
- Type I - involves ascending and descending aorta
- Type II - involves ascending aorta; associated with Marfan syndrome; least common
- Type III - involves the descending aorta (below the origin of the left subclavian artery); lowest mortality rate
- Marfan syndrome:
- Genetic disorder that affects connective tissue of the heart, vessels and bones
- Patients are usually very tall with a thin frame, long extremities and fingers
- Abraham Lincoln is believed to have had Marfan syndrome
- The aortic root and arch are the most commonly affected blood vessel (DeBakey Type II)
- Aortic dissection, aneurysm and valve insufficiency are commonly associated with this disorder
- Mitral valve prolapse and valve insufficiency are common with this disorder
Sonographic Appearance:
- Linear echogenicity seen in the lumen of the vessel, separating it into two channels; one channel is a blind ended pocket
- Color flow demonstrates two lumens, both with turbulence
- Bidirectional flow seen in false lumen




Aortic Rupture:
- Significant risk of rupture in aneurysms >7cm in diameter
- Back pain and hypotension
- Critical finding
- Varied sonographic appearance
- Irregular hypoechoic areas near an aortic aneurysm
- Hematomas can displace surrounding structures
Pseudoaneurysm:
- Caused by trauma or invasive procedures
- Blood escapes the artery into surrounding tissues and is encapsulated within the tissues
- Forms round sac of blood
- The connection with the vessel is made through a neck or stalk
- Critical finding
- Treatment by compression of the stalk or thrombin injection
- Compression performed in 10 one-minute intervals with a re-evaluation of flow with color Doppler after each compression interval
- Thrombin - clotting agent injected into a pseudoaneurysm to close the opening and clot the blood that has escaped; usually reserved for larger pseudoaneurysms with larger stalks
Sonographic Appearance:
- Rounded, anechoic structure adjacent to main artery
- Color demonstrates a connection between the artery and the structure
- Color also demonstrates turbulent flow, Yin/Yang sign within the body
- Doppler evaluation will demonstrate high resistance to-and-fro flow in the stalk and low resistance to-and-fro flow in the body


Aortic Stenosis:
- Most commonly caused by atherosclerotic changes
- Can also be related to AAA thrombosis or arteritis
- Resistance will increase proximal to the stenosis
- Causes increased velocity at the site of the stenosis
- Distal to the stenosis the flow will be dampened with tardus parvus waveforms possible
- Effects will be similar to coarctation with increased brachial pressures and decreased bilateral ankle pressures
- If the stenosis is superior to the renal artery origins, renal ischemia will activate the renin-angiotensin system causing systemic HTN
Leriche Syndrome:
- AKA aortoiliac occlusive disease
- Due to occlusion of the abdominal aorta just above the site of its bifurcation
- Causes bilateral symptoms and flow changes in the lower extremities
- Symptoms include fatigue of both lower limbs, intermittent bilateral claudication with ischemic pain, absent or diminished femoral pulses and pallor or coldness of both lower extremities
- Doppler waveforms will demonstrate low resistance, post-stenotic flow changes throughout both legs
Retroperitoneal Fibrosis:
- AKA Ormond disease
- Most commonly occurs at the level of the aortic bifurcation and inferiorly in pelvis
- Idiopathic(usually) overgrowth of fibrous tissue around an atherosclerotic aorta
- Can be related to drugs, infection, malignancy or cancer therapy
- May lead to ureteral obstruction causing hydronephrosis
- May compress the IVC causing bilateral pedal edema
- May compress the gonadal veins causing scrotal swelling
Sonographic Appearance:
- Soft tissue mass surrounding great vessels
- Hypoechoic
- Smooth borders



Available products and price list on next page
| Return to Top | Reference List |