
.jpg)
Female Breast Anatomy
Note: Click any image to enlarge.
Breast Development:
- Mammary glands begin to develop at 6wks LMP
- Multiple paired areas of ectodermal thickening occur along the mammary ridges but only one pair remains to form the breasts
- Mammary ridges are also known as milk lines
- At birth only the main lactiferous ducts have developed
- Ripening of the breast normally occurs between 9-16yrs
- Estrogen causes stromal (connective) tissue to elongate and grow, vascularity increases and fat deposition increases
- Progesterone stimulates TDLU growth
- Thelarche refers to rapid breast tissue development at puberty
- Premature Thelarche
- Refers to breast enlargement, onset of menses, underarm/pubic hair, and acne that occurs before age 8
- Most common cause is ovarian hyperstimulation due to early release of gonadotropins (luteinizing hormone and follicle stimulating hormone)
- The pituitary gland produces LH and FSH, which stimulate the ovaries
- Other causes include pituitary tumor, adrenal gland tumor and primary hypothyroidism
- Breast tissue is not considered completely mature or ripened until pregnancy and lactation occurs
- If there is no "immediate" pregnancy, the breast tissue fully matures 2 years post menarche
- Breasts are normally asymmetric in size; usually L>R
Congenital Anomalies:
- Nipple Inversion:
- Usually bilateral if congenital
- Associated with ductal ectasia and periductal mastitis
- Associated pathology can be present if the nipple change is a new finding and/or occurs unilaterally
- Athelia: absence of the nipple
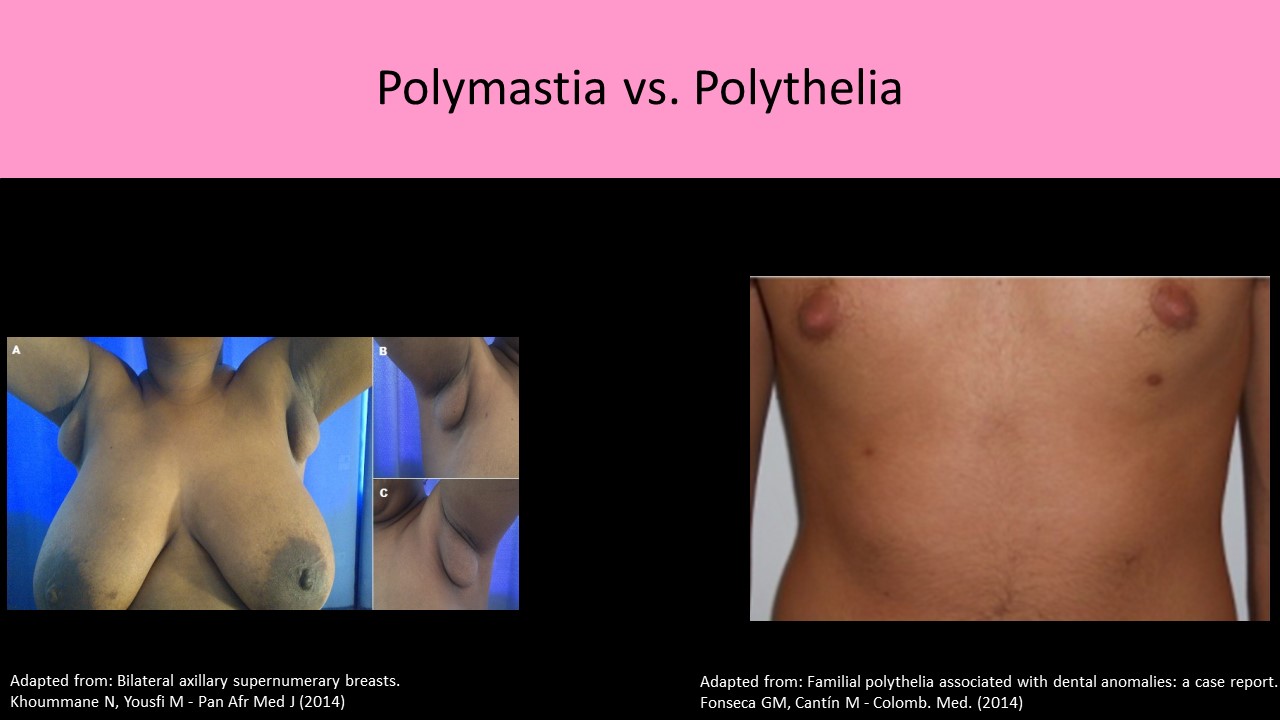
- Polythelia:
- Accessory nipples, can develop anywhere along the milk line
- Most commonly seen just inferior to the normal nipple
- #1 congenital anomaly of the breast in females and males
- Amastia: failure of the breast and nipple to develop
- Polymastia:
- Accessory breast tissue resulting from incomplete involution of mammary ridge
- Most commonly forms without a nipple
- Usually found in the axilla
- More common in men
- Amazia: absence of development of the functional breast tissue beneath a normal nipple/areola
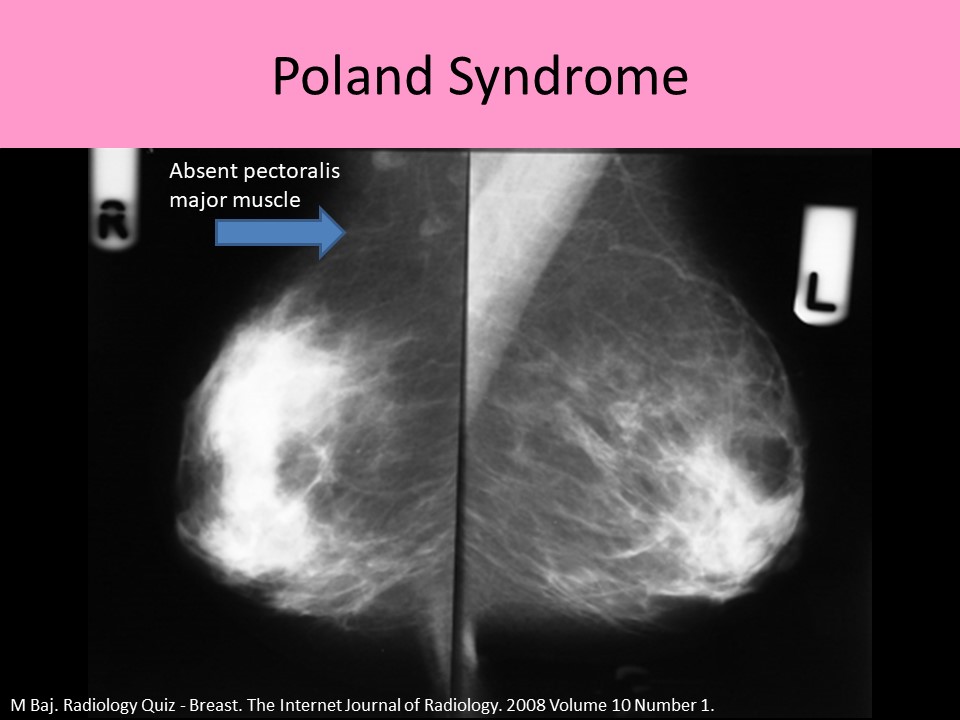
- Poland syndrome
- Missing or underdeveloped muscles on one side of the body
- Unilateral hypoplasia of breast, hemithorax, and pectoral muscle
- Upper extremity abnormalities are usually seen on the affected side
Supernumerary Breast Tissue:
- Classification developed in 1915 by Dr. Kajava
- Polymastia and/or polythelia
- Polythelia most common

Original image licensed by CC BY 2.0

Breast Anatomy:
- AKA Mammary glands
- Milk Lines: refers to the areas between the axilla and inguinal region where breast tissue may be formed
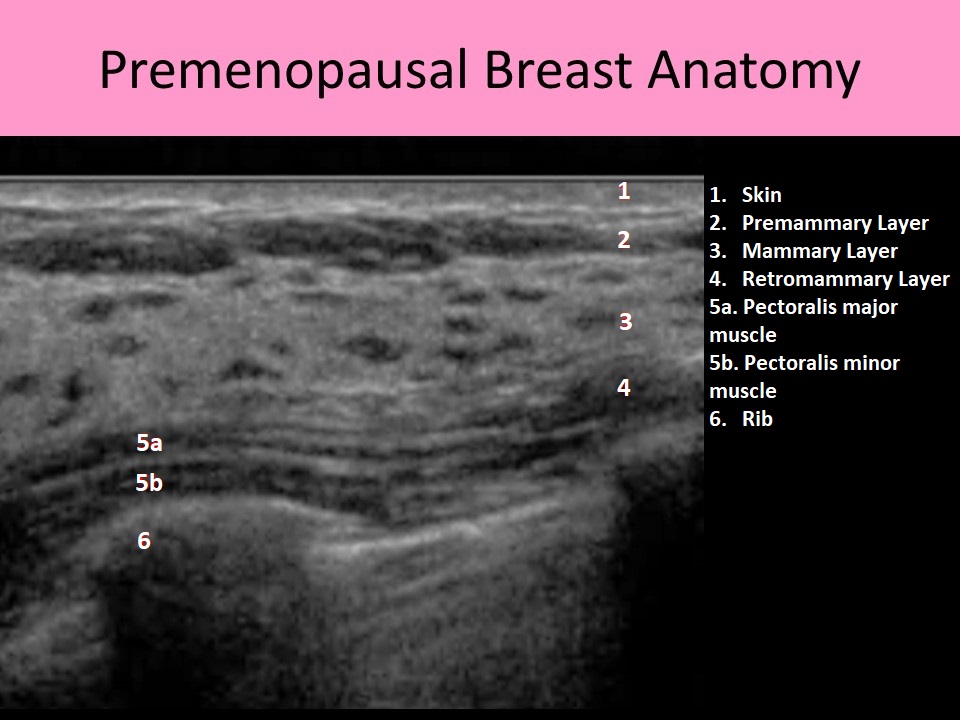
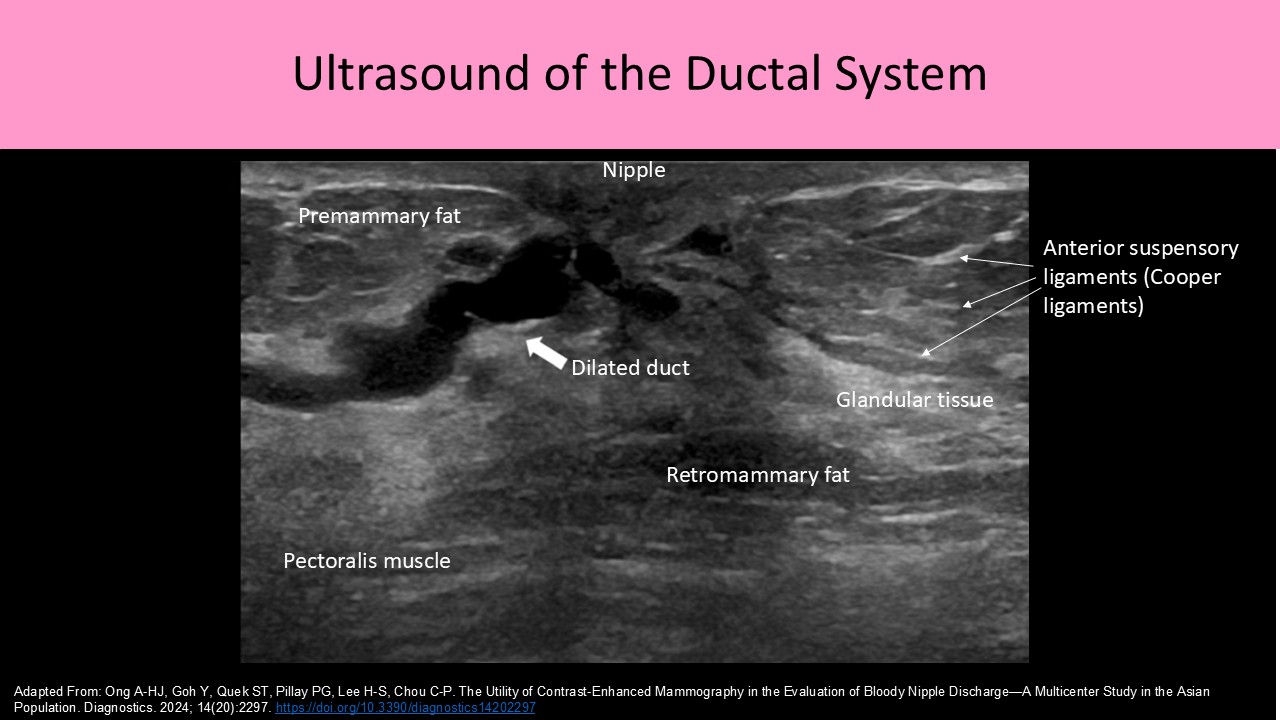
- Sonographically there are 6 layers of tissue identified:
- Skin
- Premammary layer
- Mammary layer
- Retromammary layer
- Muscle layer
- Chest wall
- Skin layer:
- Usually between 0.5 – 2mm thick
- Composed of epidermal cells
- Contains sebaceous glands and hair follicles
- Covers the subcutaneous layer of breast tissue
- Thickest at the base of the breast (inferior crease line)
- Thicker in younger patients and thins as the patient ages
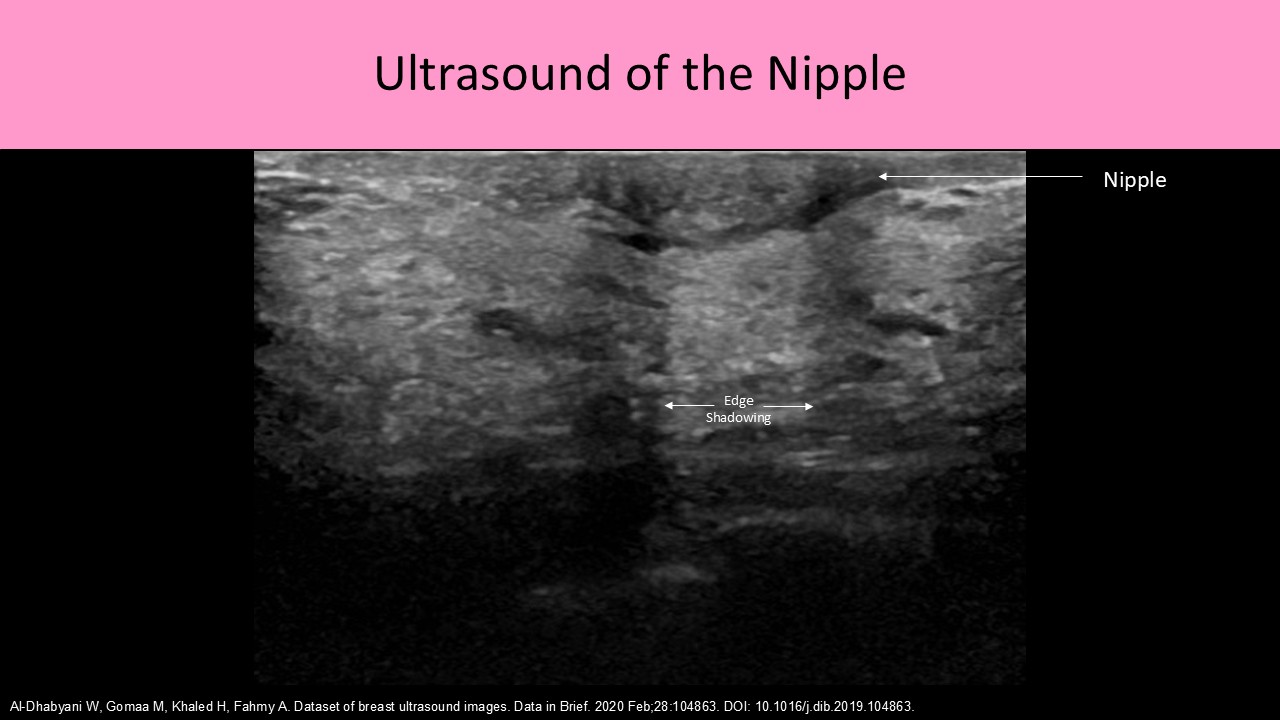
- Nipple: composed of erectile tissue and contains 15-20 small excretory ducts to drain milk
- Areola: small area of pigmented skin that encircles the nipple and is composed of smooth muscle tissue
- Montgomery glands: small sebaceous glands on the surface of the areola that secrete "protective" oily substance during lactation
- Morgagni tubercles: raised areas or bumps on the areolar region that are formed by the Montgomery gland ductal openings
- Axillary Tail of Spence: refers to the part of the mammary tissue that extends into the upper outer quadrant and axilla area
- Pectoralis muscles: lie posterior to retromammary layer and line the chest wall from the 2nd - 6th rib from sternum to axilla
- The pectoralis minor muscle lies posterior to the pectoralis major muscle
- The breast lies superior to the 7th rib and inferior to the 1st or 2nd rib
- Ribs lie posterior to the pectoralis muscles (***a rib is the most common palpable finding that is mistaken for a mass)
- Right and left intercostal nerves innervate each breast
Axilla:
- Pyramidal space directly inferior to the shoulder joint that is between the upper lateral chest and medial arm
- Contains the axillary artery and vein, brachial plexus, axillary lymph nodes and fat
- There is also possible vestigial breast glandular tissue present
- The axilla is a primary route for the spread of breast cancer
- Axilla evaluation is an important component of nodal staging
- Axillary metastases highly correlates with poor outcomes for breast cancer patients
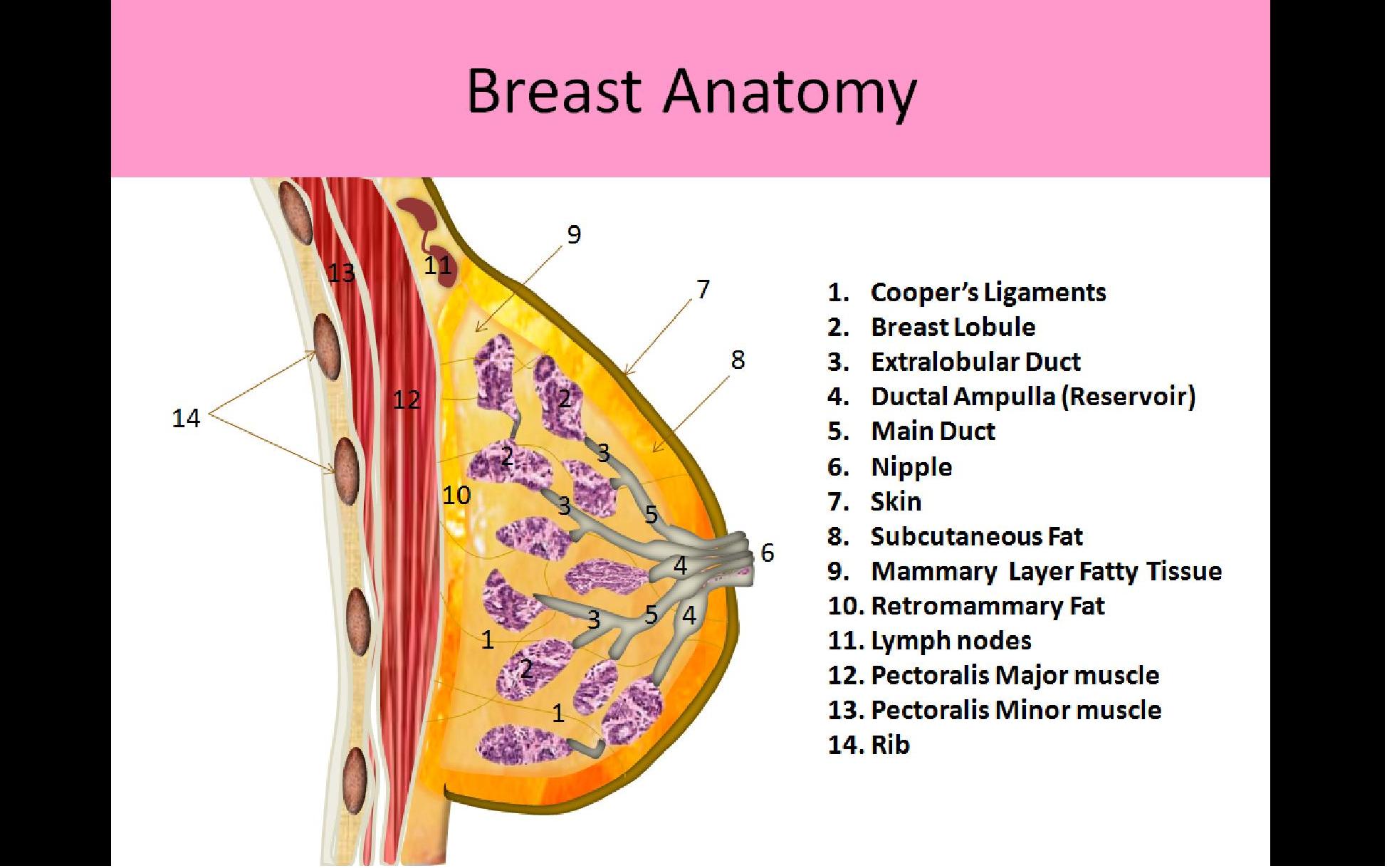

Three Layers of Breast Tissue:
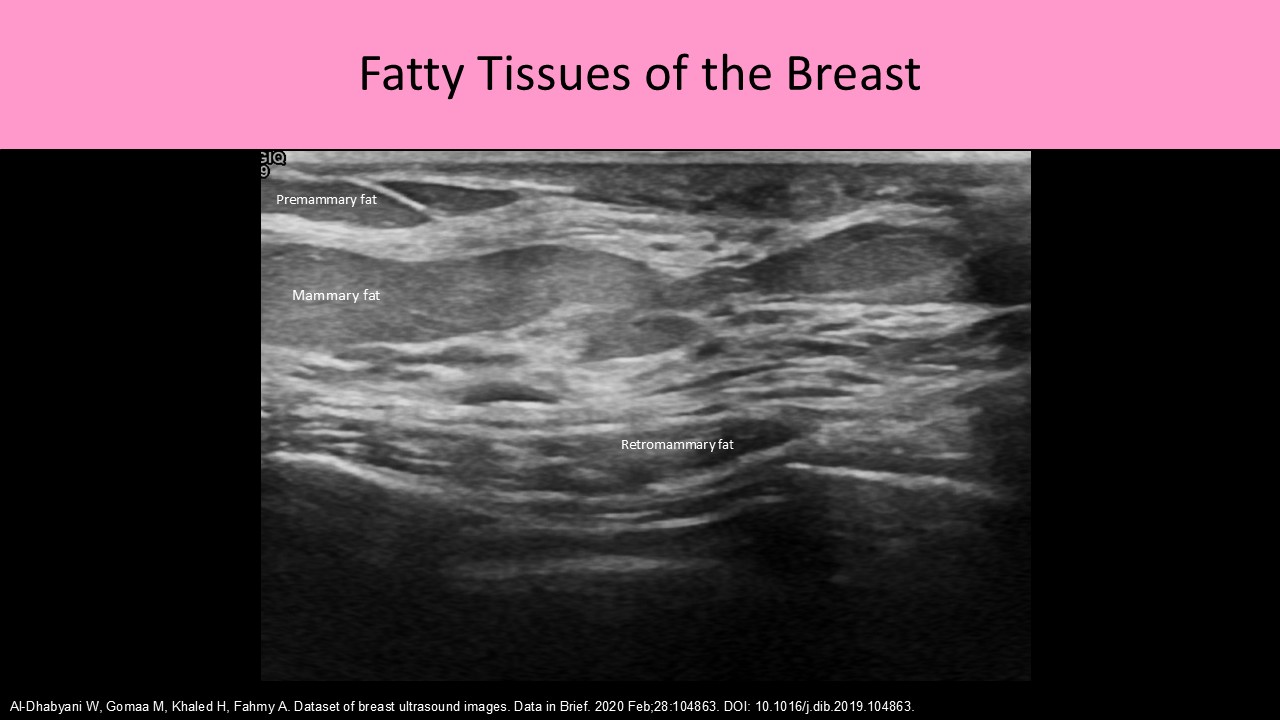
1. Premammary Layer:
- AKA subcutaneous fat layer
- Lies between the skin and the superficial layer of the superficial fascia
- Contains varied levels of fat related to age, obesity and pregnancy
- After every pregnancy, there is a reduction in breast parenchyma quantity and an increase in quantity of fat and connective tissue
- Present across the breast EXCEPT immediately posterior to the nipple
- Sebaceous cysts and lipomas occur in this layer
2. Mammary Layer
- AKA glandular or parenchymal layer
- Between the superficial and deep layers of the superficial fascia
- Only layer that contains glandular tissues (functional tissues)
- Most breast pathology originates in this layer
- Contains epithelial and stromal tissues
- Epithelial tissue is considered the functional tissue of the breast; includes TDLU, lobules, lobes, lactiferous ducts
- Stromal tissue is the structural tissue of the breast; includes fat and connective tissue
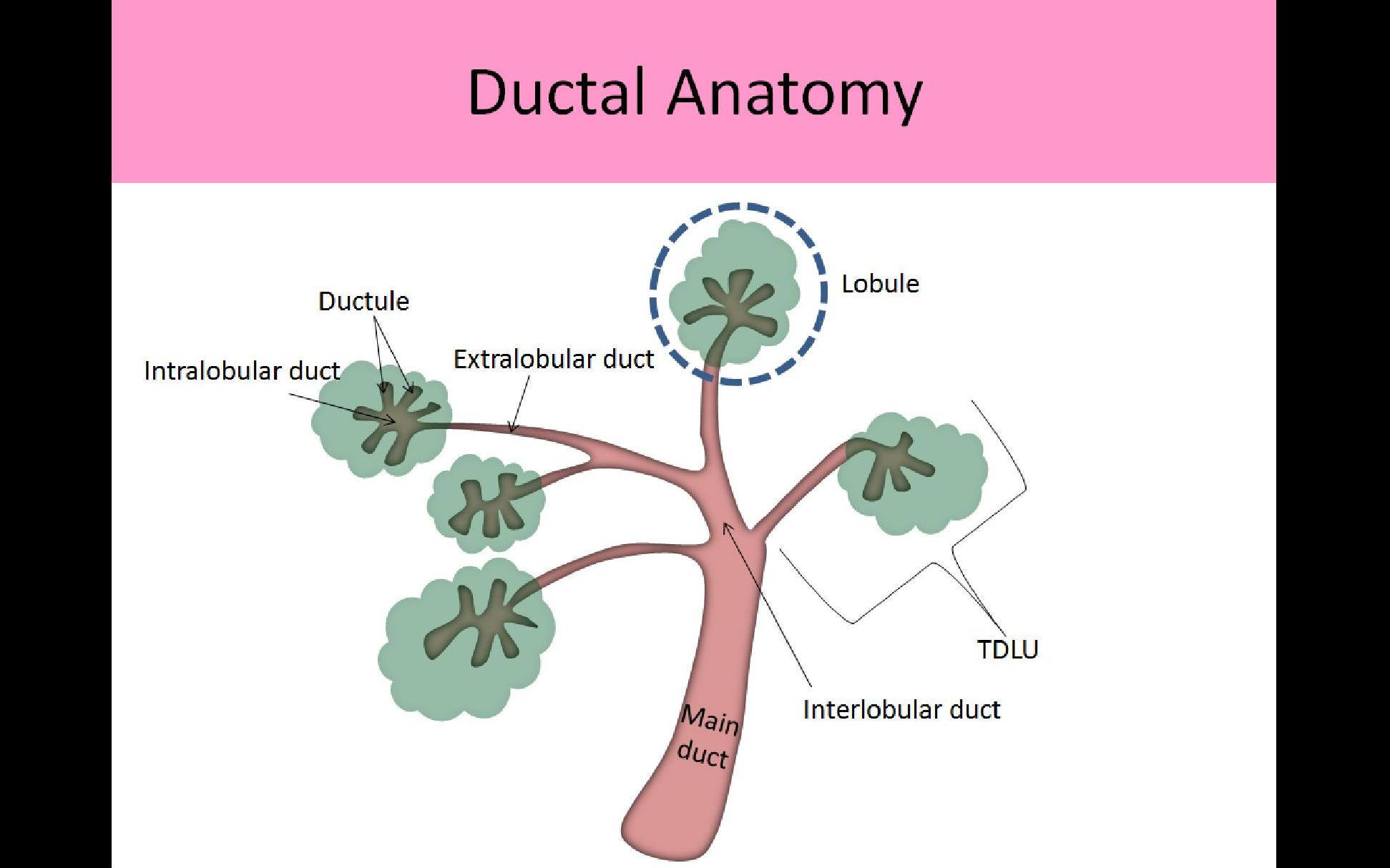
- Each breast is composed of 15-20 lobes of glandular tissue arranged in a radial fashion around the nipple and separated by fatty tissues
- Lobes consist of multiple lobules, each with an associated intralobular terminal duct
- Lobules are composed of glandular tissues which contain the functional epithelial cells (acini cells) that produce milk
- Intralobular terminal ducts from the smaller lobules drain milk into the ductal system, once the milk exits the lobule it enters the extralobular duct
- Extralobular terminal ducts converge into the main interlobular duct which drains all the milk from that cluster of lobules; end at the main extralobar duct
- Main/Extralobar ducts/Segmental ducts drain the milk from each breast lobe (15-20 ducts); ducts form a pyramid shape, focused to an apex at the areola/nipple
- Widening of the distal end of each of the main ducts is referred to as the ampulla; serves as a reservoir for milk just prior to it leaving the breast
- Interlobular/anterior suspensory/Cooper ligaments course between lobes from the deep fascia of the chest wall/axilla toward the nipple to attach to the anterior fascia of the skin
- The interlobular ligaments support the breast parenchyma
- Intralobular connective tissue is a less dense form of connective tissue that surrounds each individual lobule of breast tissue
- Upper outer quadrant of each breast contains the most glandular tissue
- The amount of glandular tissue in the mammary layer varies with age and menopause
3. Retromammary Layer:
- Located posterior to the mammary layer
- Contains varied levels of fat related to age, obesity and prior pregnancy
- After every pregnancy, there is a reduction in breast parenchyma quantity and an increase in quantity of fat and connective tissue
- Deep layer of the superficial fascia is also within the retromammary space
- This layer of tissue allows breast motion over the chest wall
Superficial Fascia:
- Surrounds all mammary tissues and separates the breast into superficial and deep tissues
- Composed of two layers; superficial and deep
- Superficial layer (superficial fascia) within the premammary layer
- The superficial layer is also called the anterior mammary fascia
- The Cooper ligaments are contiguous with the anterior mammary fascia
- Deep layer (superficial fascia) lies posterior to the mammary layer within the retromammary space
- The deep layer is also called the posterior mammary fascia
- Deep fascia lines the anterior pectoralis major muscle
- Irregularities of the deep fascia posterior to a malignancy can indicate metastasis to the chest wall


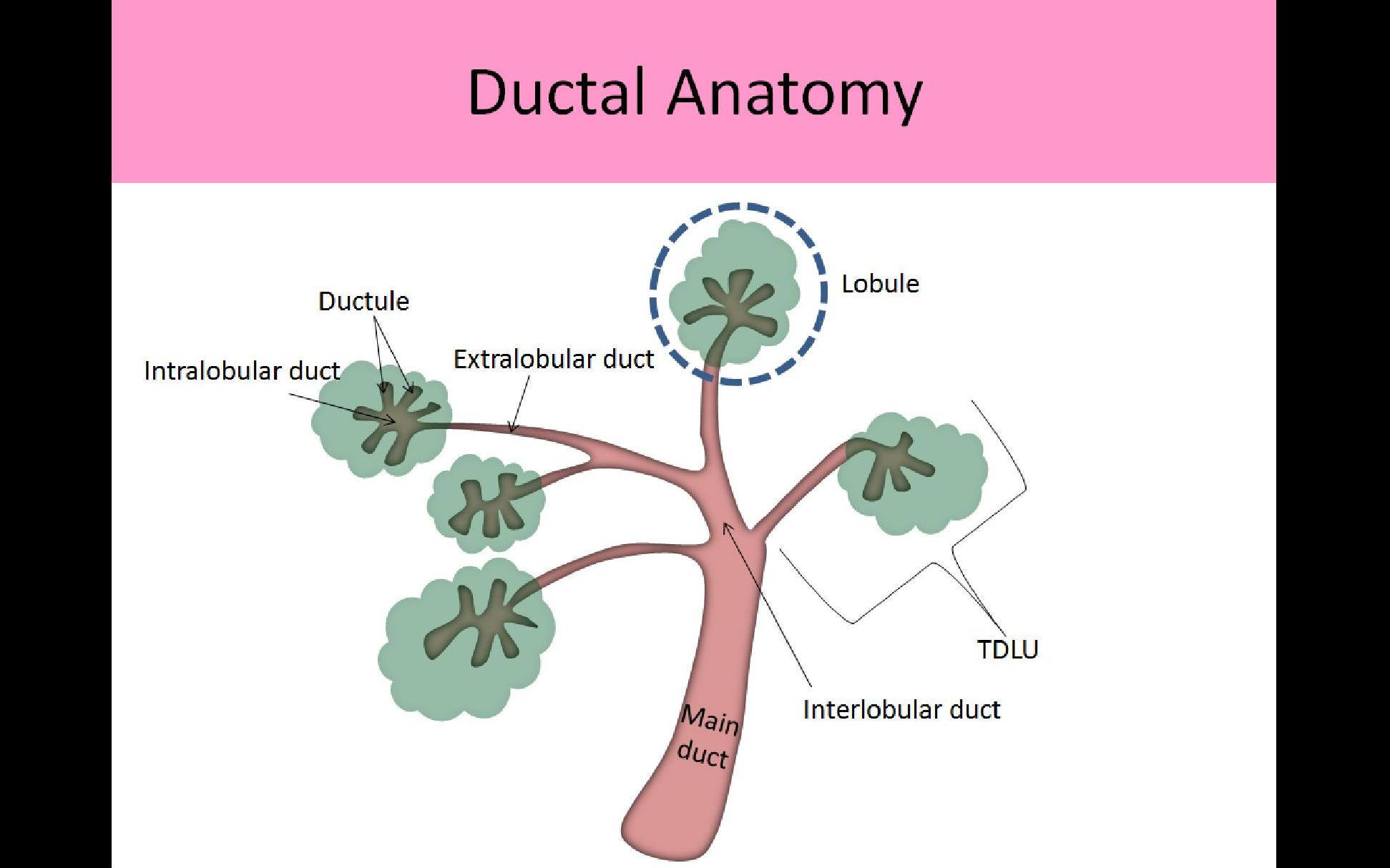
Terminal Ductolobular Unit (TDLU):
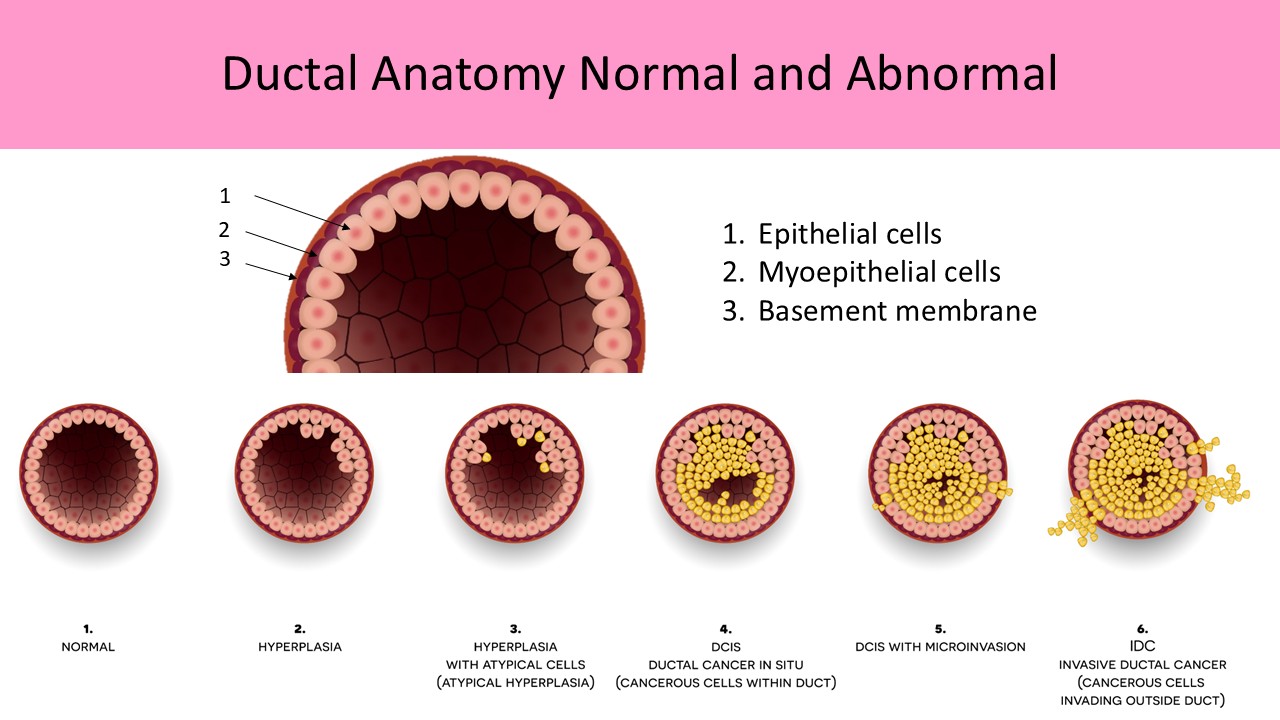
- Acini cells are the smallest functional unit of the breast
- Several hundred acini cells are in the breast
- TDLU refers to 30-50 acinar cells grouped together in a lobule and their associated terminal duct
- TDLUs are usually less than 2mm in size
- Patients with fibrocystic disease or adenosis may have up to 5mm TDLUs
- Simple cysts originate in the TDLU
- # and size of TDLUs vary with age and hormone levels
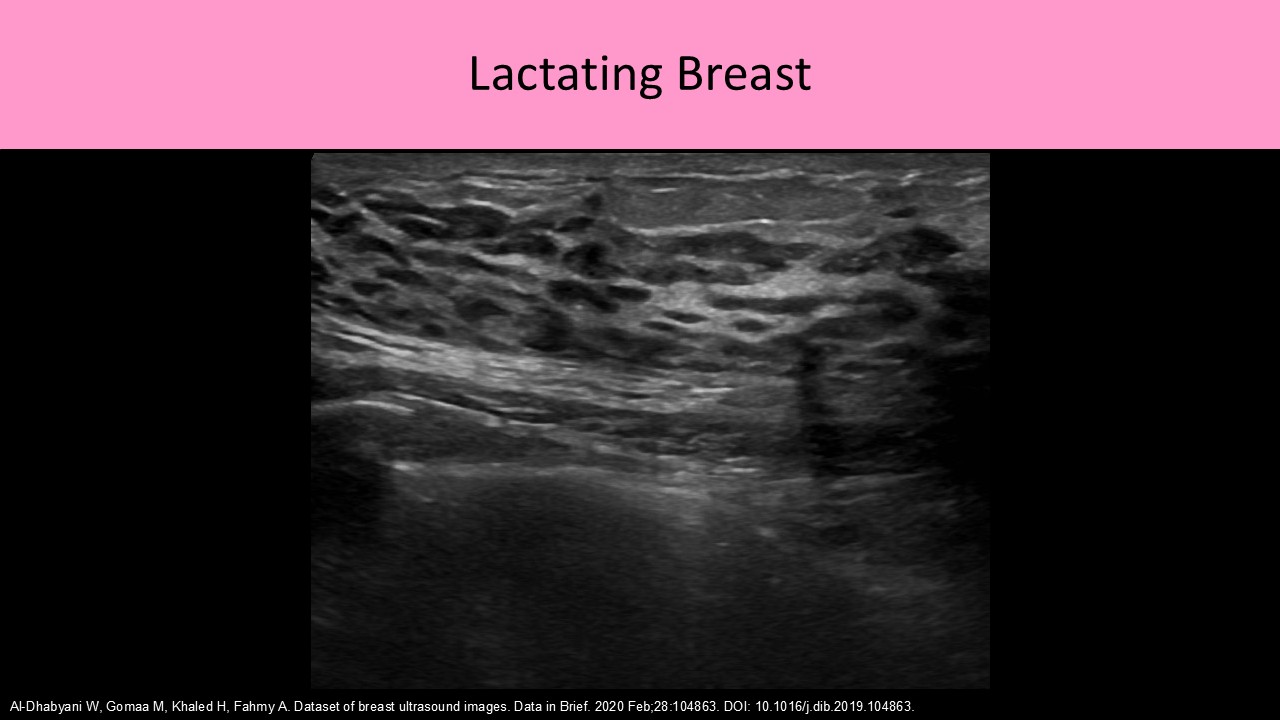
- Proliferation of the TDLUs normally occurs during reproductive years and pregnancy/lactation, also with oral contraceptives and hormone replacement therapy
- Atrophy of the breast lobules normally occurs with cessation of breast feeding and in postmenopausal women
- Nearly all breast pathology originates in the TDLU
- Most malignancies arise from the terminal duct near the junction of the intralobular and extralobular segments
- Most TDLUs are in the anterior breast, therefore most breast pathology arises in the superficial half of the mammary zone, just deep to the superficial layer of the superficial fascia
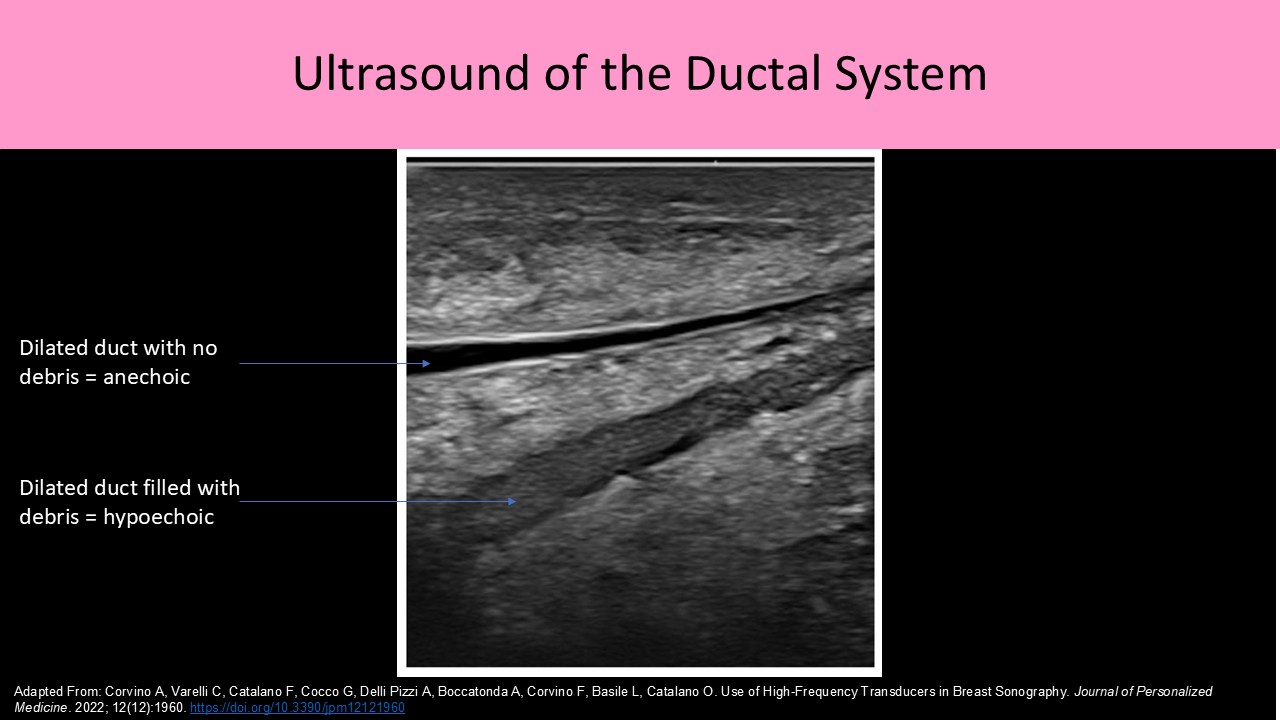
Ductal System:
- Lined with a double layer of epithelial cells to reduce friction for easier milk flow
- Middle layer composed of myoepithelial cells which aid in the movement of milk
- Basement membrane forms the outer layer of the duct which is in contact with the intralobular stroma
- Each breast lobe has one ductal system
- Normal ducts in a non-lactating female should measure <2mm diameter and increase in size closer to the nipple
- Normal ducts in a lactating female should measure <8mm diameter
- Each terminal duct begins within the lobule and extends to the nipple
- Intralobular terminal ducts - carry milk from the acini
- Extralobular terminal ducts - once the milk exits the lobule it enters the Extralobular duct
- Interlobular terminal ducts - extralobular ducts converge into the main Interlobular duct; travel between the breast lobules to reach the main extralobar duct
- Main Extralobar Ducts/Main Terminal Ducts/Segmental Ducts - drain the milk from each breast lobe; end at the ampulla
- Lactiferous Sinus or Ampulla which is an area of ductal enlargement just prior to the opening to the nipple; usually 2-3mm in diameter indicates a normal finding
- Collection ducts or Excretory ducts - 15-20 openings that excrete the milk from the nipple
- Nipple
Vasculature:
Arterial Supply:
- Lateral thoracic artery:
- Originates from the axillary artery and courses lateral and inferior along the pectoralis major muscle
- Courses from the axilla to the nipple
- Supplies lateral breast tissues
- Internal thoracic artery (AKA internal mammary artery)
- Originates at the subclavian artery
- Courses lateral to the sternum
- Supplies medial breast tissues
- Used for coronary bypass surgery when other vessels unavailable (great saphenous vein, radial artery)
- Thoracoacromial artery supplies superior breast tissue
- Intercostal artery supplies the inferior breast tissue
- There are 18 intercostal arteries on each side of the spine
- They course between the ribs and branches supply the breast with oxygenated blood
Venous Drainage:
- Lymphatic drainage pathways parallel venous drainage
- Superficial venous system lies within the subcutaneous fat tissue
- There are usually no accompanying arteries for the superficial veins of the breast
- Blood moves from the superficial system into the deep system
- Most distal veins line the superficial fascia and drain blood centrally
- Provides connection between right and left breast with potential for metastasis to occur between breasts
- Deep venous system consists of veins that follow the arterial system
- These veins typically have an accompanying artery on their course
- Primary route of venous drainage of the breast
- Includes internal mammary vein, lateral thoracic, axillary, subclavian and intercostal veins
- Drain into the axillary vein, subclavian vein and SVC

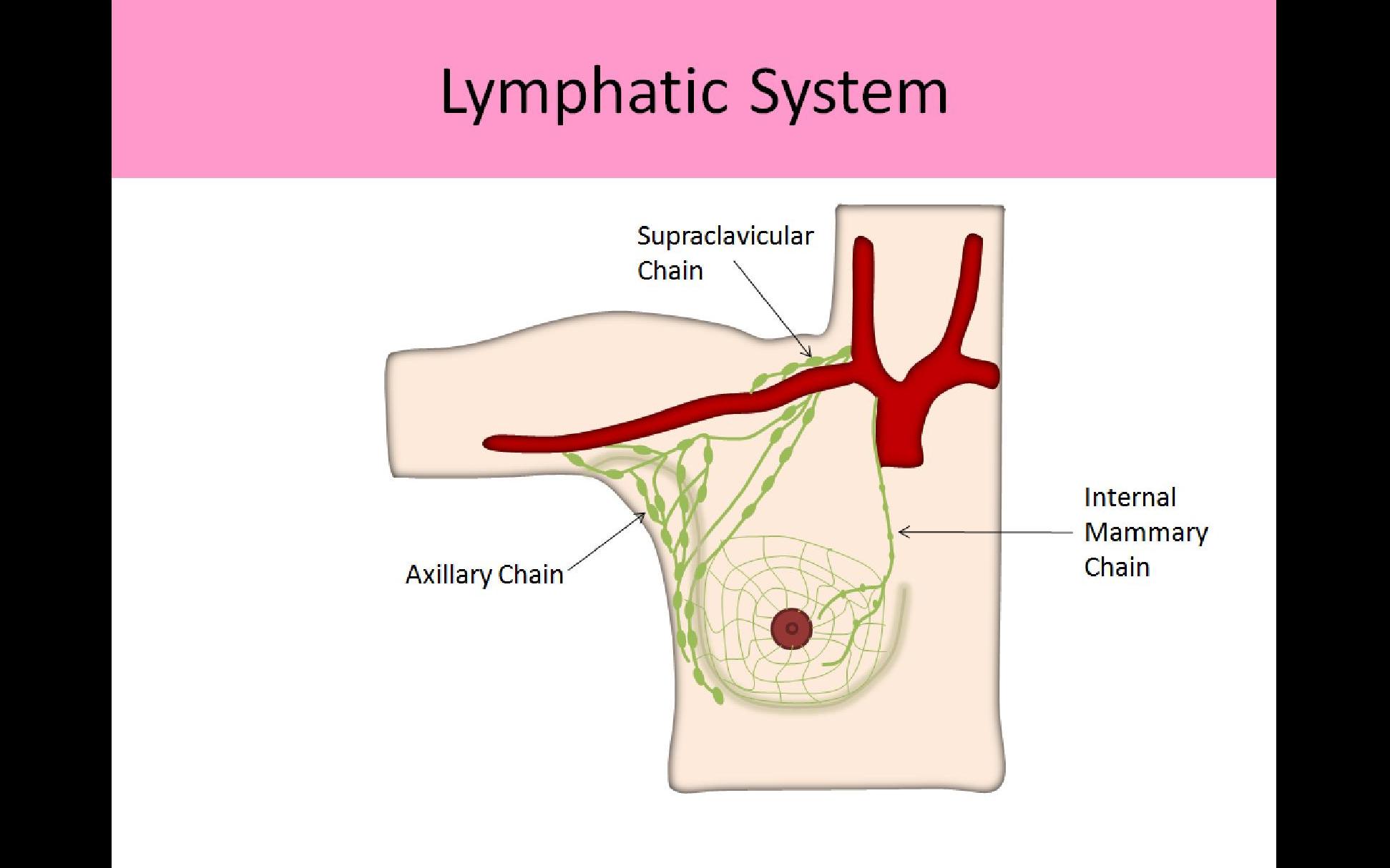
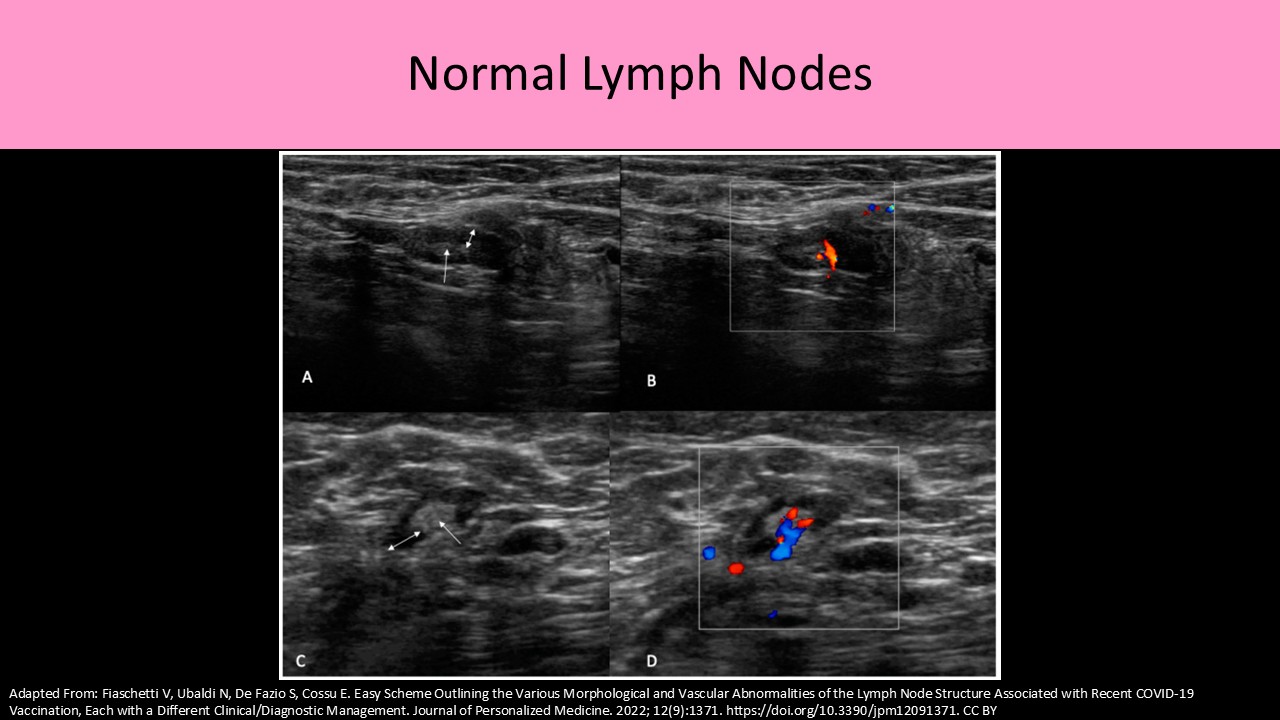
Lymphatic System:
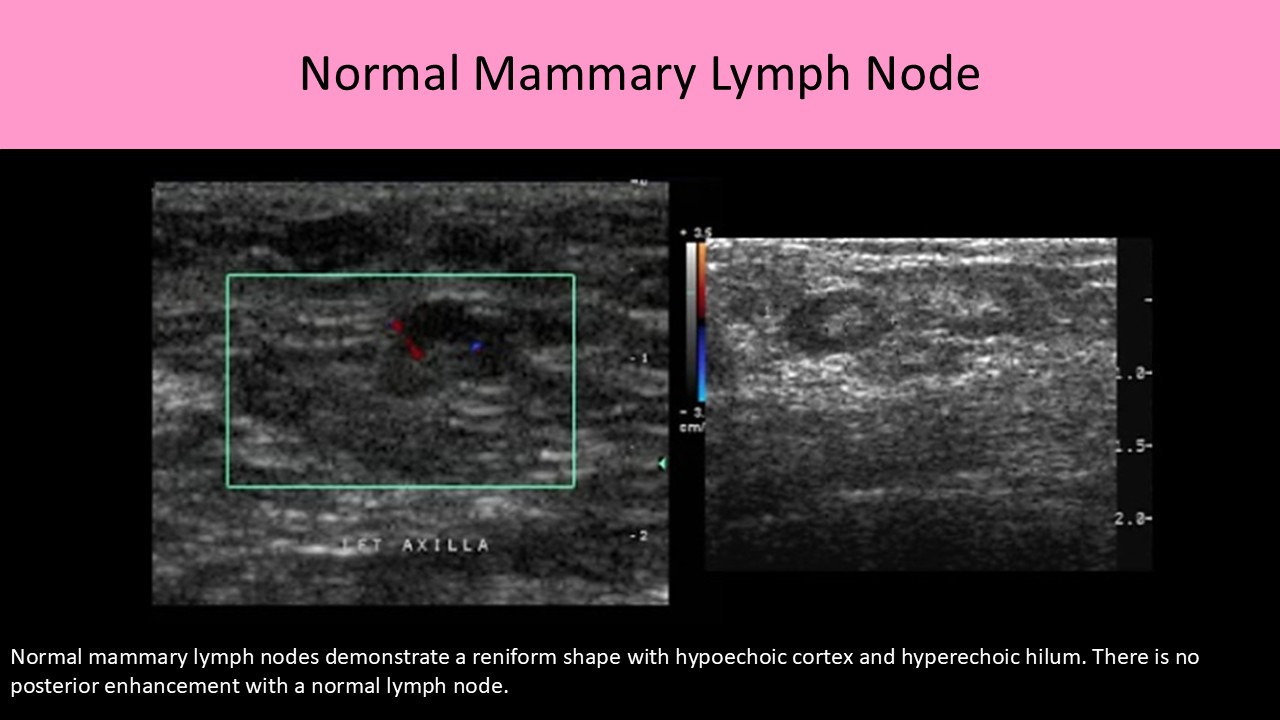
- Intramammary nodes are found within the breast parenchyma
- They are normally oval or reniform (kidney-shaped) in shape
- Lymph nodes are most concentrated in the upper outer quadrants
- Lymph vessels closely follow the venous drainage system of the breast
- Lymphatic system function is important for assessing possible routes for metastasis
- Superficial lymphatic vessels drain the lymph from the skin layer
- Deep lymphatic vessels drain the lymph from the breast tissue, nipple and areola
- Flow in the deep lymph system travels toward the areola and superficial system
- Most lymphatic drainage moves from deep to superficial, which is opposite of the venous drainage system of the breast where blood moves from the superficial system to the deep system
- Flow in the superficial system moves centrally toward the nipple
- Once the lymph fluid reaches the subareolar plexus, it then moves toward the axilla
- Majority of lymph flow out of the breast occurs through the axillary chain (75%)
- A smaller amount drains through the internal mammary and intercostal lymphatic chains
- Lymphatic vessels contain valves to assist in the flow of lymphatic fluid
- Lymphatic vessels are not usually visible Sonographically
- Lymphatic vessels do not easily dilate when flow abnormalities are present and they are not easily compressible when dilated
- The lymphatic system of the breast is the primary route of spread of breast cancer
- Lymphatic channels may communicate with the contralateral skin and breast
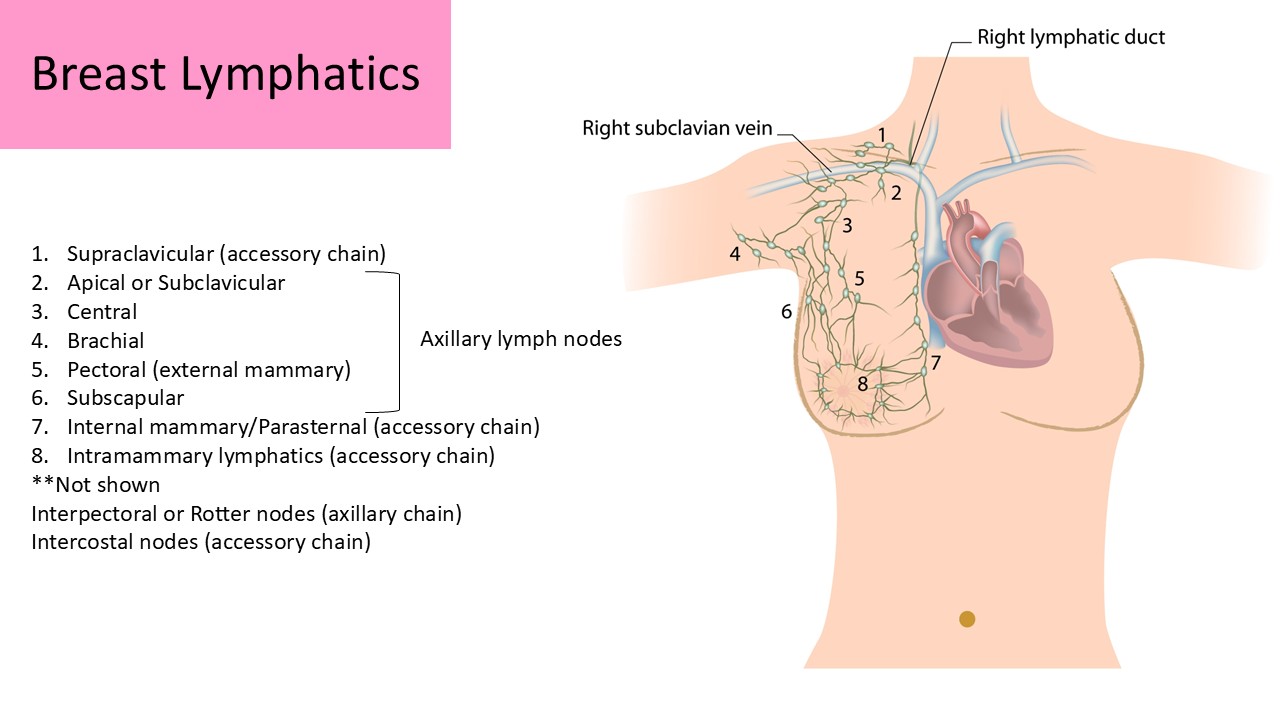
Axillary Lymph Node Categories:
- Lymph nodes and vessels that follow the course of the lateral axillary vessels
- Consists of 30-40 lymph nodes responsible for 75% of lymph drainage
- #1 site for lymph node metastasis from breast cancer
- Drains the lateral half of the breast and tail of Spence (internal mammary chain drains the medial breast)
- Subclavicular or Apical: segment that follows the course of the subclavian vessels
- Central: segment located within fatty tissues medial to the axillary vessels
- Brachial: segment lateral to the axilla in the arm
- External Mammary (pectoral): segment that follows the course of the lateral thoracic vessels, nodes are typically within a centimeter from the blood vessels
- Subscapular: segment that follows the course of the subscapular vessels
- Rotter nodes (interpectoral): segment located between the pectoral major and minor muscles
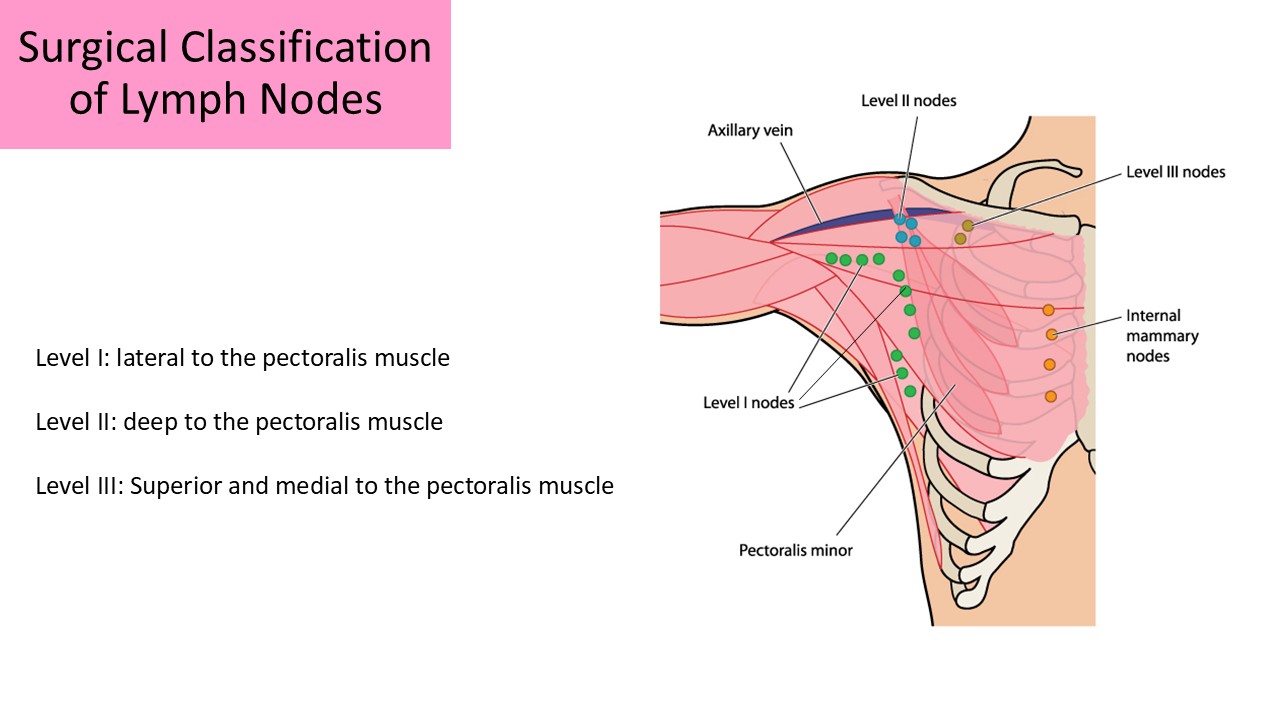
Axillary Node Classification:
- Used for staging and developing the surgical approach
- Lymph nodes are grouped according to their location relative to the pectoralis minor muscle
- Nodes are assessed for metastasis
- Lymph drainage to the axilla passes through level I, then level II and finally to level III
- The sentinel node is usually a level I node
Level I - found in nodes lateral to pectoralis minor muscle; pectoral, subscapular, lateral, and paramammary nodes
Level II - found in nodes deep to the pectoralis minor muscle; interpectoral (Rotter) and central nodes
Level III - found in nodes medial to the pectoralis minor muscle; apical nodes
Accessory Node Chains (25%)
- Intramammary: within the glandular tissue of the breast
- Internal Mammary or Parasternal:
- Lymph nodes and vessels that follow the internal mammary (internal thoracic) vessels
- Drains the medial breast
- Involved in metastatic drainage most commonly with medial cancer formation
- Intercostal: found along the intercostal arteries as the course between the ribs
- Supraclavicular:
- Found adjacent to the internal jugular vein and the subclavian vein
- Only involved in metastasis if level I, II and II nodes are affected
- Considered distant metastasis and if involved, the prognosis is very poor
- 3 primary nerve groups of the breast: Medial, lateral, and superior mammary branches
- Medial and lateral branches originate from branches of 2nd-6th intercostal nerves
- Superior branches originate from the supraclavicular branches of cervical plexus
- 2nd intercostal nerve innervates axillary tail and may be injured during axillary nodal dissection