.jpg)
Female Breast Anatomy
Note: Click any image to enlarge.
Breast Development:
- Mammary glands begin to develop at 6wks LMP
- Multiple paired areas of ectodermal thickening occur along the mammary ridges but only one pair remains to form the breasts
- Mammary ridges are also known as milk lines
- At birth only the main lactiferous ducts have developed
- Ripening of the breast normally occurs between 9-16yrs
- Estrogen causes stromal (connective) tissue to elongate and grow, vascularity increases and fat deposition increases
- Progesterone stimulates TDLU growth
- Thelarche refers to rapid breast tissue development at puberty
- Premature Thelarche
- Refers to breast enlargement, onset of menses, underarm/pubic hair, and acne that occurs before age 8
- Most common cause is ovarian hyperstimulation due to early release of gonadotropins (luteinizing hormone and follicle stimulating hormone)
- The pituitary gland produces LH and FSH, which stimulate the ovaries
- Other causes include pituitary tumor, adrenal gland tumor and primary hypothyroidism
- Breast tissue is not considered completely mature or ripened until pregnancy and lactation occurs
- If there is no "immediate" pregnancy, the breast tissue fully matures 2 years post menarche
- Breasts are normally asymmetric in size; usually L>R
Congenital Anomalies:
- Nipple Inversion: usually bilateral if congenital; associated pathology can be present if the nipple change is a new finding and/or occurs unilaterally
- Athelia: absence of the nipple
- Polythelia: accessory nipples, can develop anywhere along the milk line; most commonly seen just inferior to the normal nipple; #1 congenital anomaly of the breast in females and males
- Amastia: failure of the breast and nipple to develop
- Polymastia: accessory breast tissue; most commonly forms without a nipple; usually found in the axilla
- Amazia: absence of development of the functional breast tissue beneath a normal nipple/areola
Supernumerary Breast Tissue:
- Classification developed in 1915 by Dr. Kajava
- Polymastia and/or polythelia
- Polythelia most common
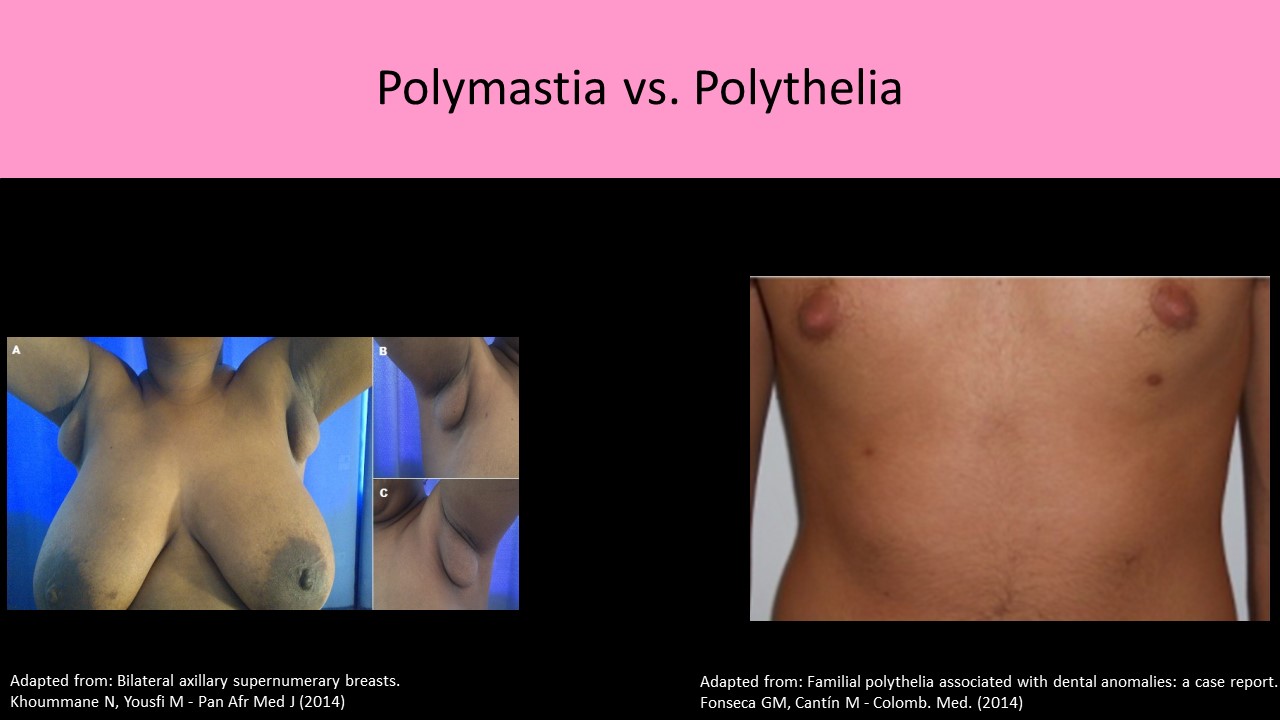
Original image licensed by CC BY 2.0
Breast Anatomy:
- AKA Mammary glands
- Milk Line: AKA mammary ridges refers to the area between the axilla and inguinal region where breast tissue may be formed, EX: Accessory nipples
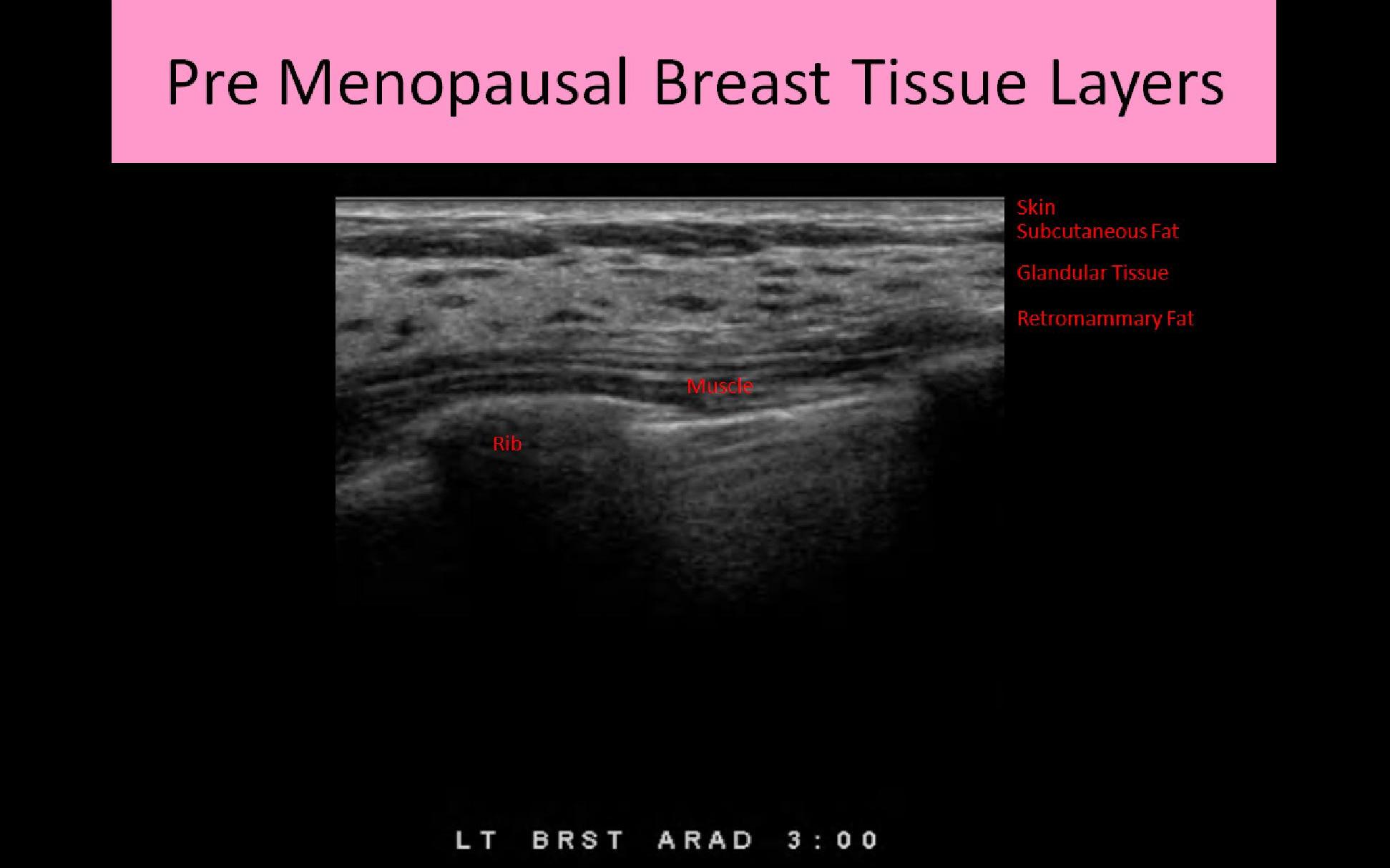
- Sonographically there are 6 layers of tissue identified:
- skin
- premammary layer
- mammary layer
- retromammary layer
- muscle layer
- chest wall
- Skin layer:
- Usually between 0.5 – 2mm thick
- Composed of epidermal cells
- Contains sebaceous glands and hair follicles
- Covers the subcutaneous layer of breast tissue
- Thickest at the base of the breast (inferior crease line)
- Thicker in younger patients and thins as the patient ages
- Nipple: composed of erectile tissue and contains small excretory ducts to drain milk
- Areola: small area of pigmented skin that encircles the nipple; composed of smooth muscle tissue
- Montgomery glands: small sebaceous glands on the surface of the areola that secrete "protective" oily substance during lactation
- Axillary Tail of Spence refers to the part of the mammary tissue that extends into the upper outer quadrant and axilla area
- Pectoralis muscles lie posterior to retromammary layer and line the chest wall from the 2nd - 6th rib from sternum to axilla
- The pectoralis minor muscle lies posterior to the pectoralis major muscle
- The breast lies superior to the 7th rib and inferior to the 1st or 2nd rib
- Ribs lie posterior to the pectoralis muscles; a rib is the most common palpable finding that is mistaken for a mass
- Right and left intercostal nerves innervate each breast
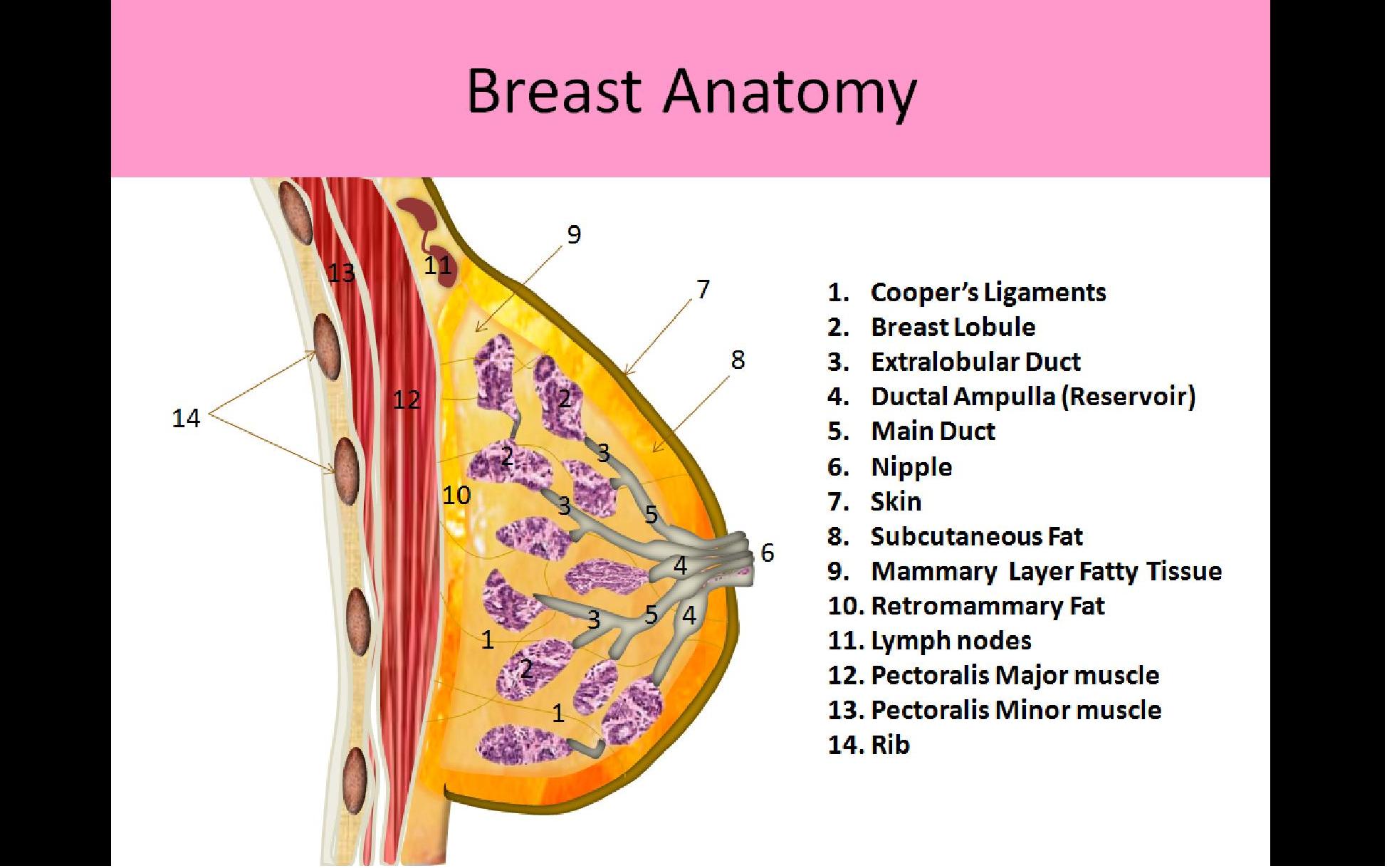
Three Layers of Breast Tissue:
1. Premammary Layer:
- AKA subcutaneous fat layer
- Lies between the skin and the superficial layer of the superficial fascia
- Contains varied levels of fat related to age, obesity and pregnancy
- Present across the breast EXCEPT immediately posterior to the nipple
- Sebaceous cysts and lipomas occur in this layer
2. Mammary Layer
- AKA glandular or parenchymal layer
- Between the superficial and deep layers of the superficial fascia
- Only layer that contains glandular tissues (functional tissues)
- Most breast pathology originates in this layer
- Contains epithelial and stromal tissues
- Epithelial tissue is considered the functional tissue of the breast includes TDLU, lobules, lobes, lactiferous ducts
- Stromal Tissue is the structural tissue of the breast includes fat and connective tissue
- Each breast is composed of 15-20 lobes of glandular tissue arranged in a radial fashion around the nipple and separated by fatty tissues
- Lobes consist of multiple lobules each with an associated intralobular duct
- Lobules are composed of glandular tissues which contain the functional epithelial cells (acini cells) that produce milk
- Intralobular terminal ducts from the smaller lobules drain milk into the ductal system, once the milk exits the lobule it enters the extralobular duct
- Extralobular terminal ducts converge into the main interlobular duct which drains all the milk from that cluster of lobules; end at the main extralobar duct
- Main/Extralobar ducts drain the milk from each breast lobe (15-20 ducts); ducts form a pyramid shape, focused to an apex at the areola/nipple
- Main ducts drain the milk from each breast lobe (15-20 ducts); ducts form a pyramid shape, focused to an apex at the areola/nipple
- Widening of the distal end of each of the main ducts is referred to as the ampulla; serves as a reservoir for milk just prior to it leaving the breast
- Cooper’s ligaments course between lobes from the chest wall/axilla toward the nipple to support the breast parenchyma; AKA interlobular connective tissue
- Intralobular connective tissue is a less dense form of connective tissue that surrounds each individual lobule of breast tissue
- Upper outer quadrant of each breast contains the most glandular tissue
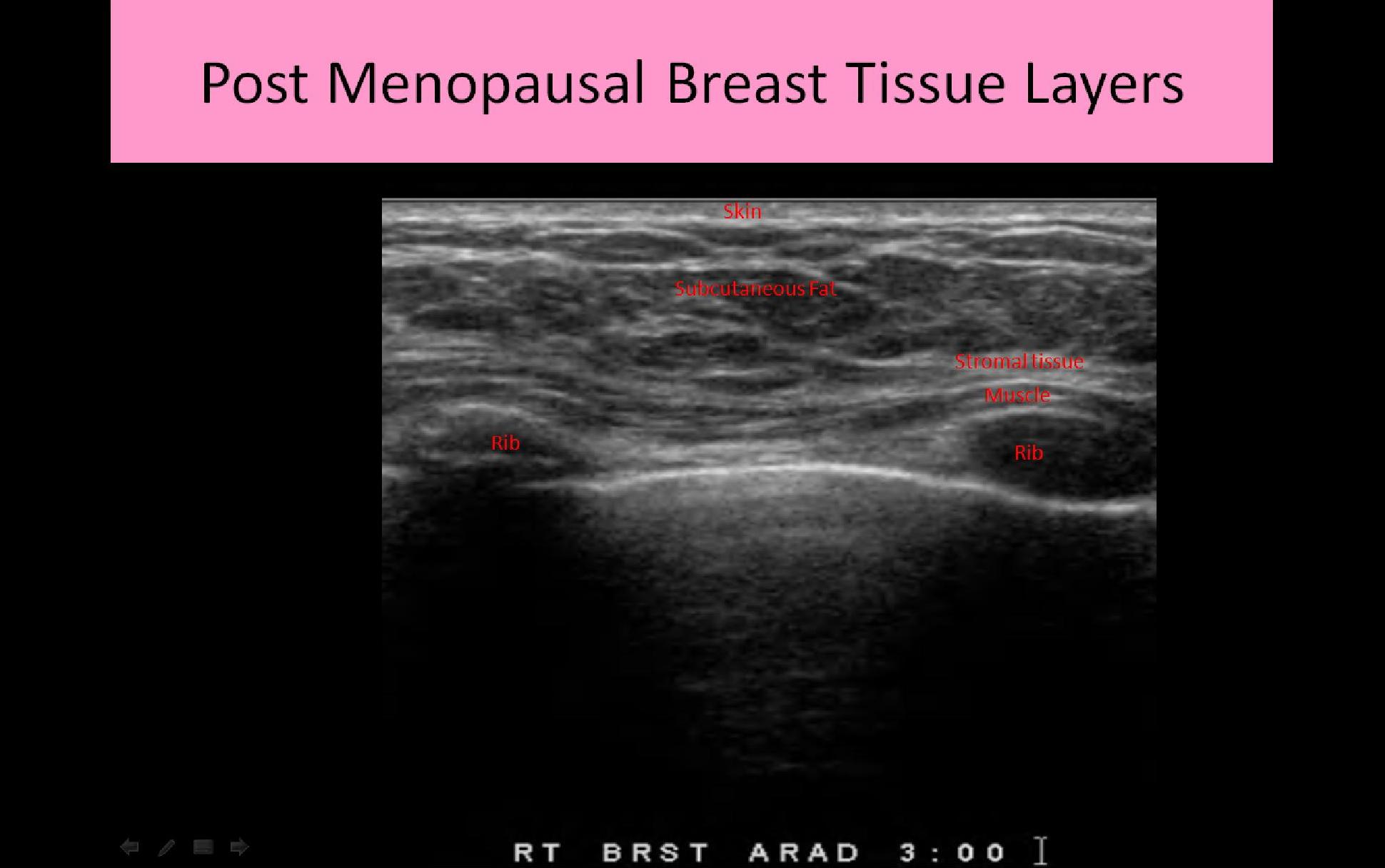
- The amount of glandular tissue in the mammary layer varies with age and menopause
3. Retromammary Layer:
- Located posterior to the mammary layer
- Contains varied levels of fat related to age, obesity and pregnancy
- Deep fascia also within the retromammary space
- This layer of tissue allows breast motion over the chest wall
Superficial Fascia:
- Surrounds all mammary tissues and separates the breast into superficial and deep tissues
- Composed of two layers; superficial and deep
- Superficial layer (superficial fascia) within the premammary layer
- Deep layer (deep fascia) lies posterior to the mammary layer within the retromammary space
- Irregularities of the deep fascia posterior to a malignancy can indicate metastasis to the chest wall
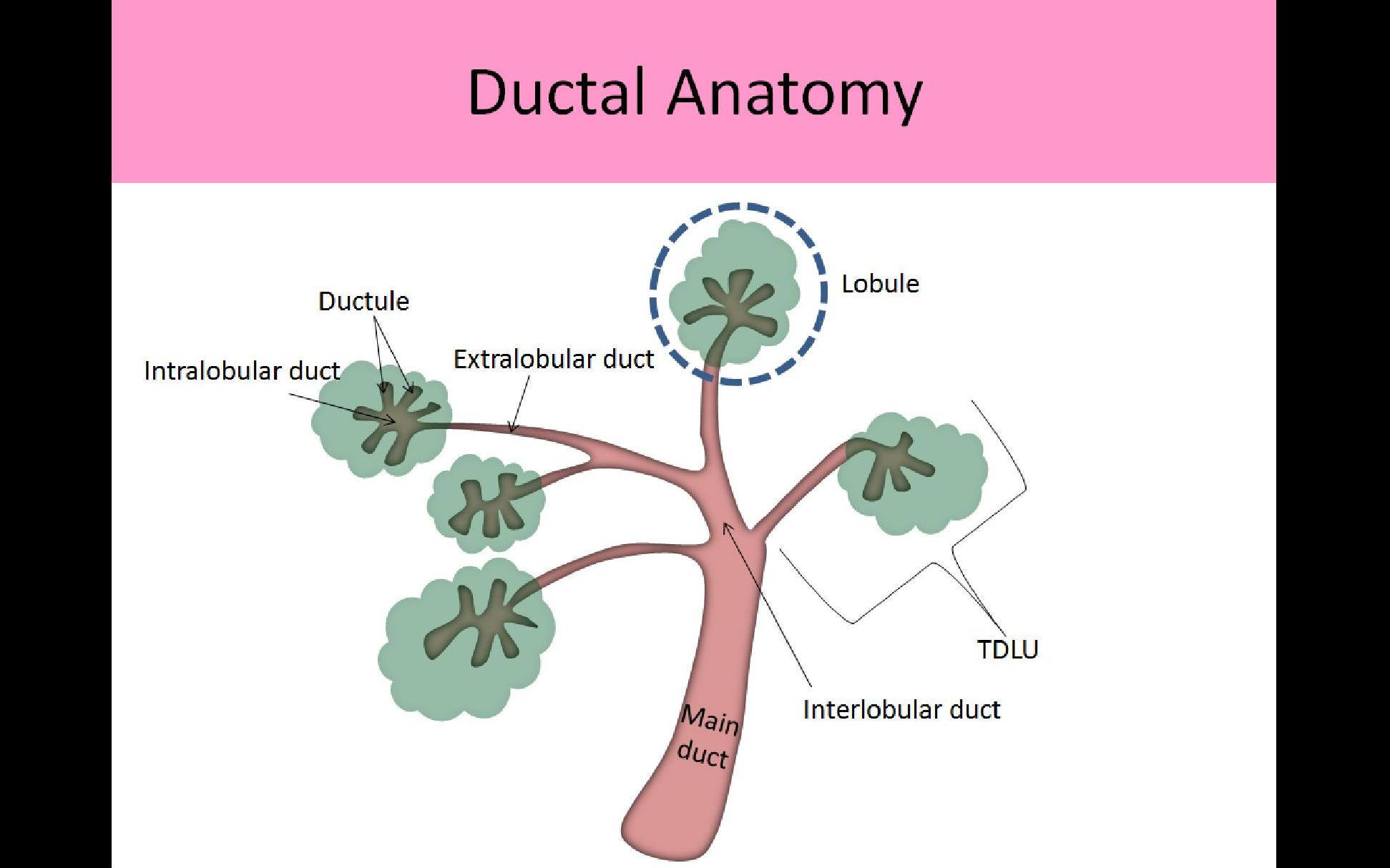
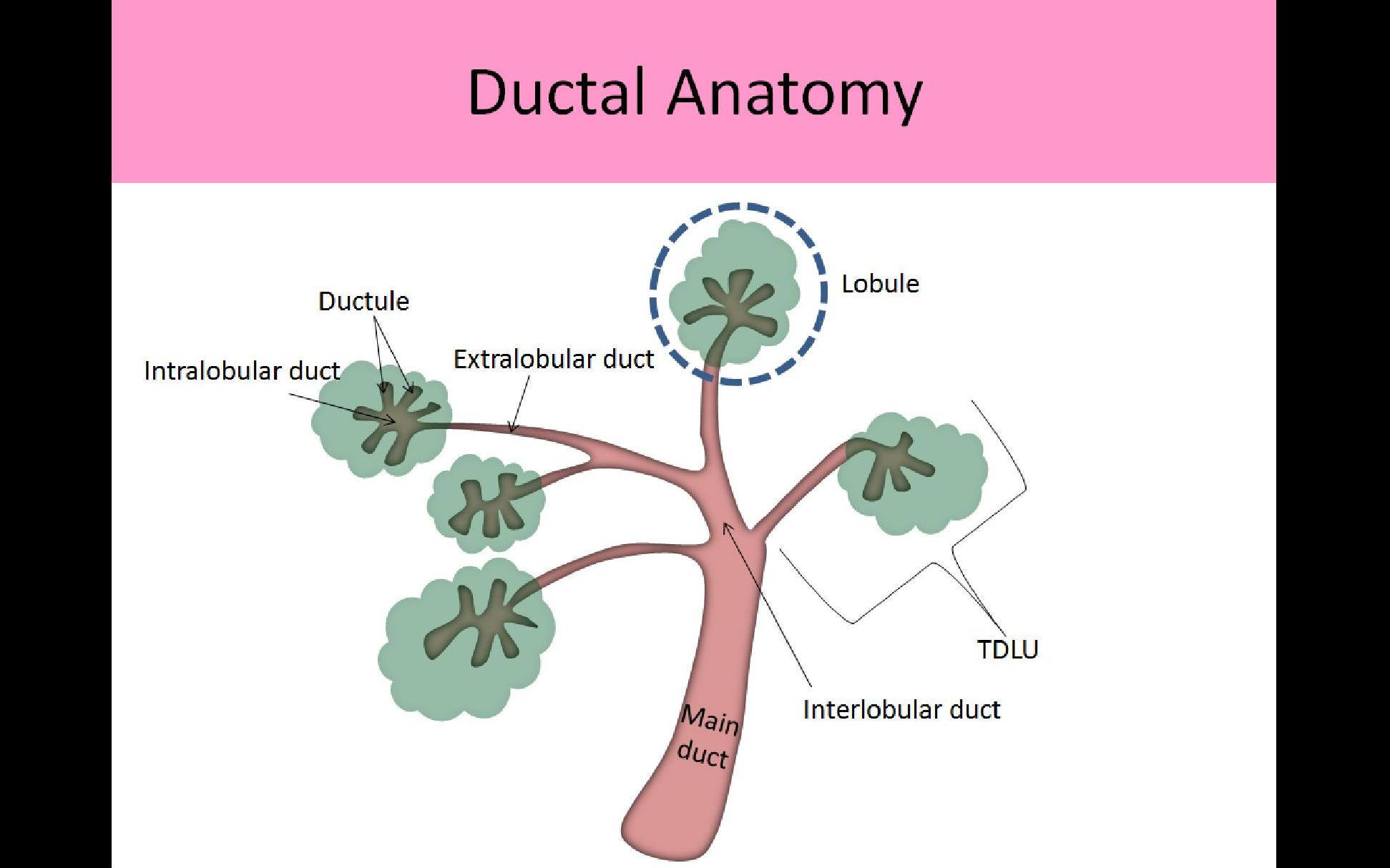
Terminal Ductolobular Unit (TDLU):
- Acini cells are considered the "functional unit" of the breast
- Several hundred acini cells are in the breast
- TDLU refers to 30-50 acinar cells grouped together in a lobule and their associated terminal duct
- Acini cells are the smallest functional unit of the breast
- TDLU usually less than 2mm in size
- Patients with fibrocystic disease or adenosis may have up to 5mm TDLUs
- # and size of TDLUs vary with age and hormone levels
- Proliferation of the TDLUs normally occurs during reproductive years and pregnancy/lactation
- Atrophy of the breast lobules normally occurs with cessation of breast feeding and in postmenopausal women
- Nearly all breast pathology originates in the TDLU
- Most malignancies arise from the terminal duct near the junction of the intralobular and extralobular segments
- Most TDLUs are in the anterior breast, therefore most breast pathology arises in the superficial half of the mammary zone, just deep to the superficial layer of the superficial fascia
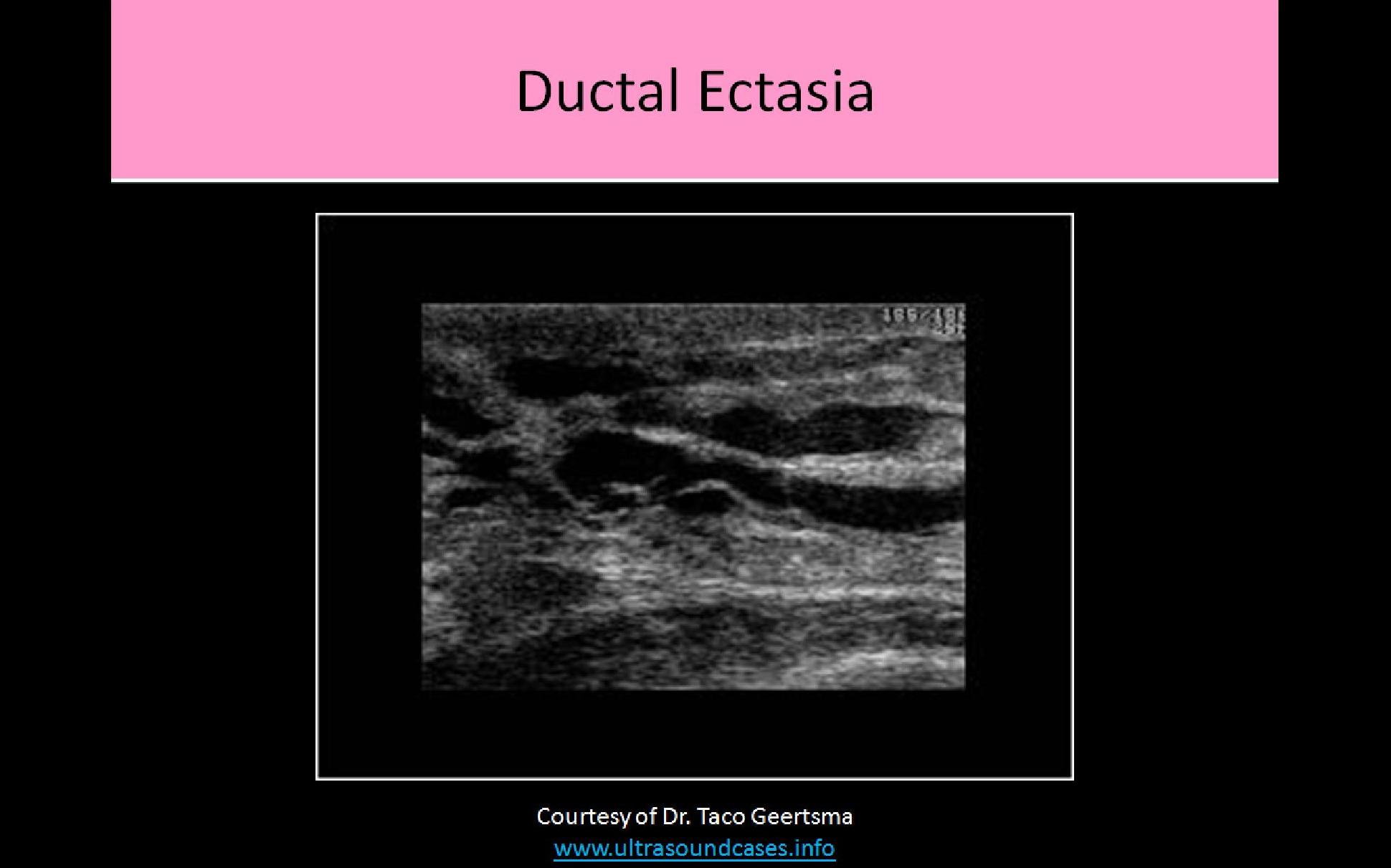
Ductal System:
- Lined with epithelial cells to reduce friction for easier milk flow
- Middle layer composed of myoepithelial cells which aids in the movement of milk
- Basement membrane forms the outer layer of the duct which is in contact with the intralobular stroma
- Each breast lobe has one ductal system
- Normal ducts in a non-lactating female should measure <2mm diameter and increase in size closer to the nipple
- Normal ducts in a lactating female should measure <8mm diameter
- Each terminal duct begins within the lobule and extends to the nipple
- Intralobular terminal ducts - carry milk from the acini
- Extralobular terminal ducts - once the milk exits the lobule it enters the Extralobular duct
- Interlobular terminal ducts -Extralobular ducts converge into the main Interlobular duct; travel between the breast lobules to reach the main extralobar duct
- Main Extralobar Ducts/Main Terminal Ducts - drain the milk from each breast lobe; end at the ampulla
- Lactiferous Sinus or Ampulla which is an area of ductal enlargement just prior to the opening to the nipple; usually 2-3mm in diameter indicates a normal finding
- Collection ducts or Excretory ducts - 15-20 openings that excrete the milk from the nipple
- Nipple
Vasculature:
Arterial Supply:
- Lateral thoracic artery:
- Originates from the axillary artery and courses lateral and inferior along the pectoralis major muscle
- Supplies lateral breast tissues
- Internal thoracic artery (AKA internal mammary artery)
- Originates at the subclavian artery
- Courses lateral to the sternum
- Supplies medial breast tissues
- Used for coronary bypass surgery when other vessels unavailable (great saphenous vein, radial artery)
- Thoracoacromial artery supplies superior breast tissue
- Intercostal artery supplies the inferior breast tissue
Venous Drainage:
- Superficial venous system lies within the subcutaneous fat tissue
- Blood moves from the superficial system into the deep system
- Most distal veins line the superficial fascia and drain blood centrally
- Provides connection between right and left breast with potential for metastasis to occur between breasts
- Deep venous system consists of veins that follow the arterial system
- Primary route of venous drainage of the breast
- Communicates with the axillary vein, subclavian vein and SVC
- Includes internal mammary vein, lateral thoracic, axillary, subclavian and intercostal veins
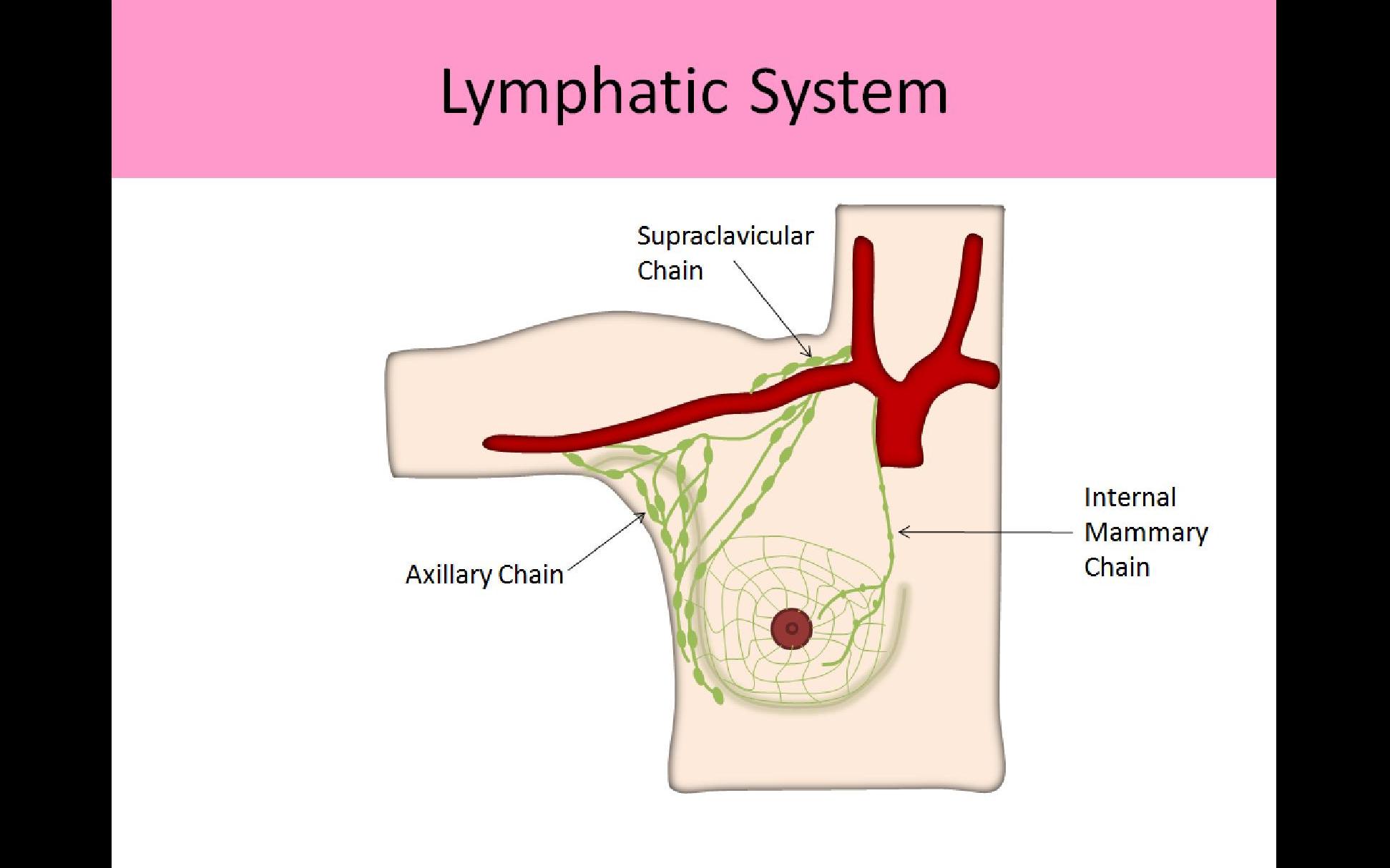
Lymphatic System:
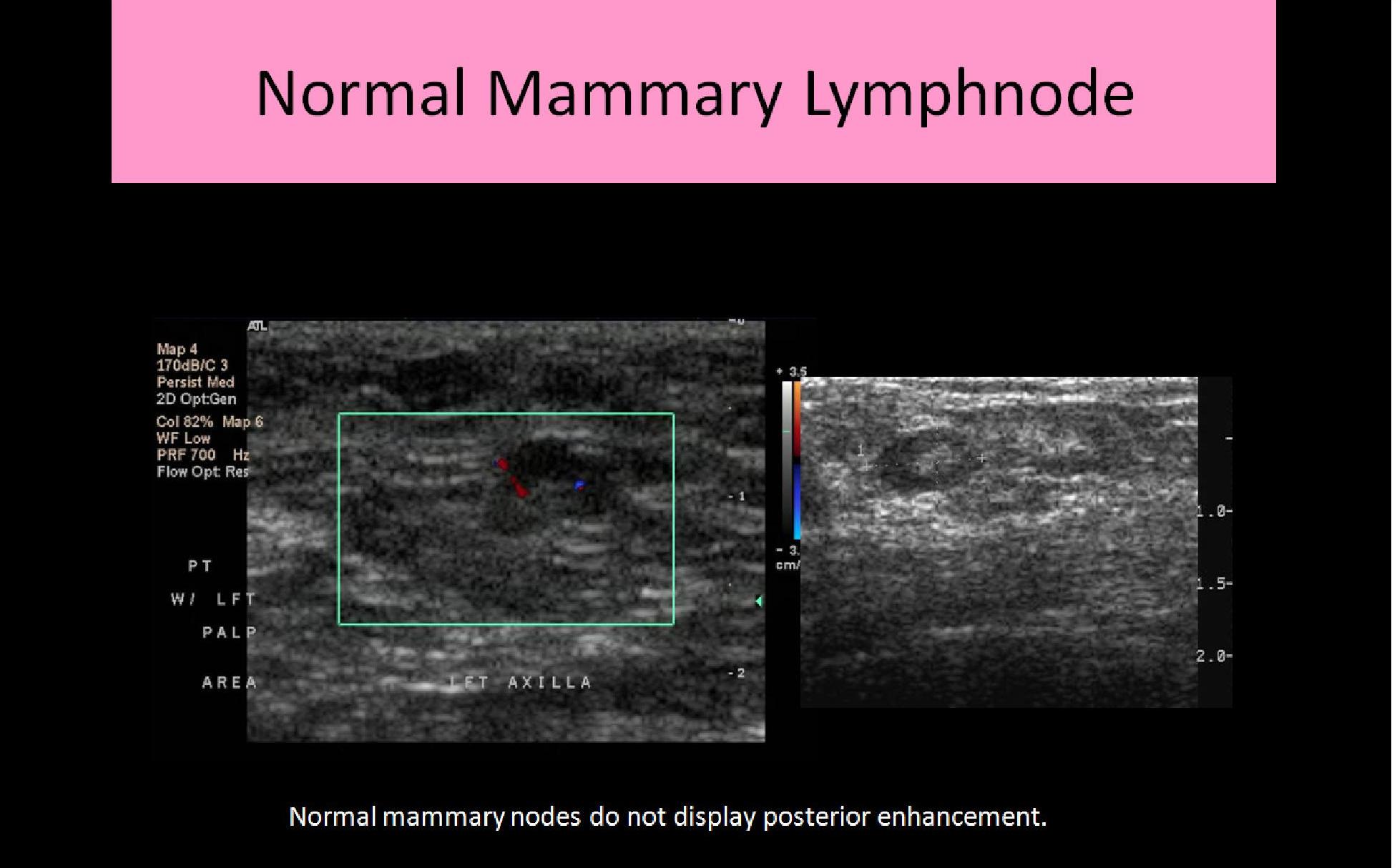
- Intramammary nodes are found within the breast parenchyma
- Lymph nodes are most concentrated in the upper outer quadrants
- Lymph vessels closely follow the venous drainage system of the breast
- Lymphatic system function is important for assessing possible routes for metastasis
- Superficial lymphatic vessels drain the lymph from the skin layer
- Deep lymphatic vessels drain the lymph from the breast tissue, nipple and areola
- Flow in the deep lymph system travels toward the areola and superficial system
- Most lymphatic drainage moves from deep to superficial, which is opposite of the venous drainage system of the breast where blood moves from the superficial system to the deep system
- Flow in the superficial system moves centrally toward the nipple
- Once the lymph fluid reaches the subareolar plexus, it then moves toward the axilla
- Majority of lymph flow out of the breast occurs through the axillary (75%)
- A smaller amount drains through the internal mammary and intercostal lymphatic chains
- Lymphatic vessels contain valves to assist in the flow of lymphatic fluid
- Lymphatic vessels are not usually visible Sonographically
- Lymphatic vessels do not easily dilate when flow abnormalities are present and they are not easily compressible when dilated
Lymphatic Chains Draining the Breast:
- External Mammary: segment that follows the course of the lateral thoracic vessels
- Scapular: segment that follows the course of the subscapular vessels
- Axillary: lymph nodes and vessels that follow the course of the lateral axillary vessels; consists of 30-40 lymph nodes responsible for 75% of lymph drainage; #1 site for lymph node metastasis from breast cancer
- Subclavicular: segment that follows the course of the subclavian vessels
- Central: segment located within fatty tissues medial to the axillary vessels
- Rotter’s (interpectoral): segment located between the pectoral major and minor muscles
Axillary Node Classification:
- Used for staging and developing the surgical approach
- Lymph nodes are grouped according to their location relative to the pectoralis minor muscle
- Nodes are assessed for metastasis
- Lymph drainage to the axilla passes through level I, then level II and finally to level III
- The sentinal node is usually a level I node
Level I - found in nodes lateral to pectoralis minor muscle; pectoral, subscapular, lateral, and paramammary nodes
Level II - found in nodes deep to the pectoralis minor muscle; interpectoral and central nodes
Level III - found in nodes medial to the pectoralis minor muscle; apical nodes
Accessory Node Chains (25%)
- Intramammary: usually lie within a centimeter of the posterior mammary artery that extends from the axilla to the nipple
- Internal Mammary: lymph nodes and vessels that follow the internal mammary vessels; involved in metastatic drainage most commonly with medial cancer formation
- Intercostal/Parasternal: found adjacent to the course of the internal thoracic artery and vein
- Supraclavicular - found adjacent to the internal jugular vein and the subclavian vein; only involved in metastasis if level I, II and II nodes are affected; considered distant mestastasis and if involved, the prognosis is very poor
Breast Physiology:
- Exocrine gland - secretes substance carried by a ductal system (milk)
- Main function is the production and secretion of milk
- Acini cells are the smallest functional unit of the breast
- Several hundred acini cells in each breast produce milk into a separate duct (terminal duct)
- Milk funneled into the ductal system toward the nipple
- Estrogen - produced by the ovaries; levels rise during the first half of the menstrual cycle and stimulate ductal proliferation
- Progesterone - produced by the ovaries; levels rise with ovulation and stimulate lobular proliferation and growth which can lead to "PMS" symptoms in breasts
- Prolactin inhibitors - produced by the hypothalamus; prevents lactation until pregnancy
- Prolactin - produced by the pituitary gland; stimulates milk production with pregnancy
- Oxytocin - produced by the pituitary gland; causes ductal contraction with lactation
- Estrogen and progesterone levels decrease significantly after birth and prolactin levels increase to stimulate milk production
- Milk production usually begins within 2-3 days post-partum
Breast Tissue Changes:
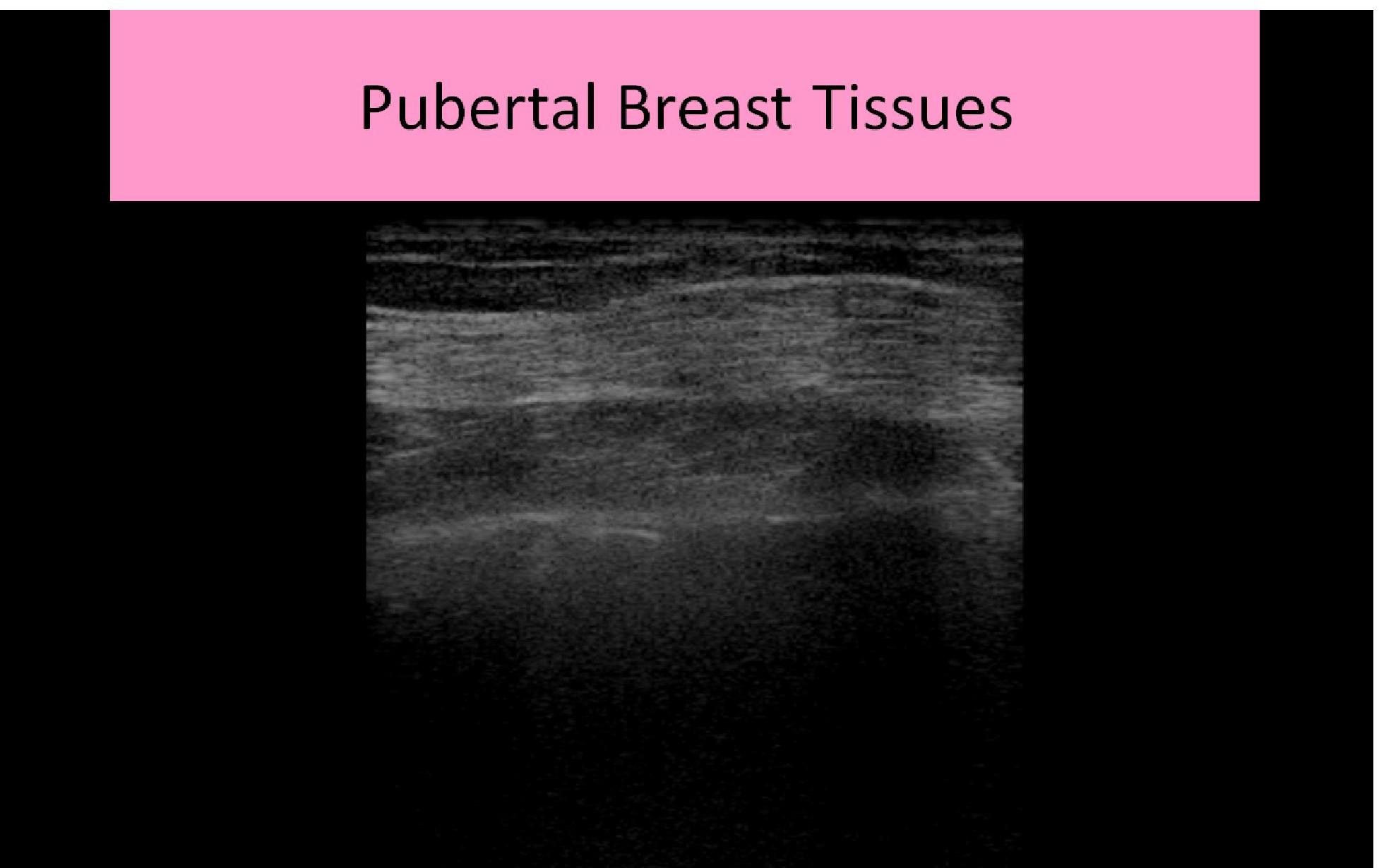
- Puberty: estrogen and progesterone stimulate breast development
- Pregnancy: acinar cells are stimulated by prolactin to produce milk while oxytocin causes ductal contraction during infant suckling; breasts enlarge due to engorgement of ducts with milk
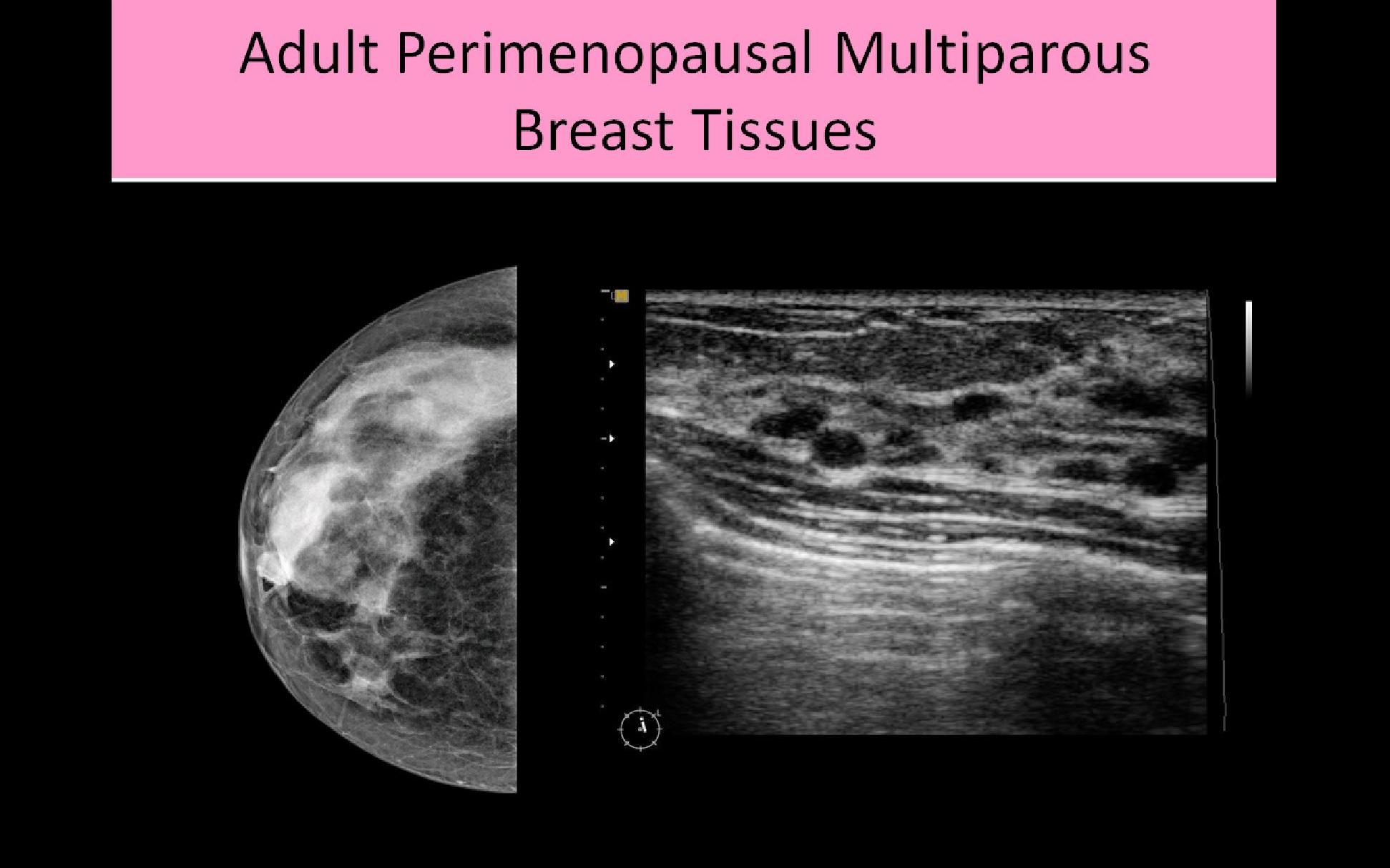
- Perimenopausal: Hormone levels decrease, glandular tissue shrivels or involutes, fat levels increase
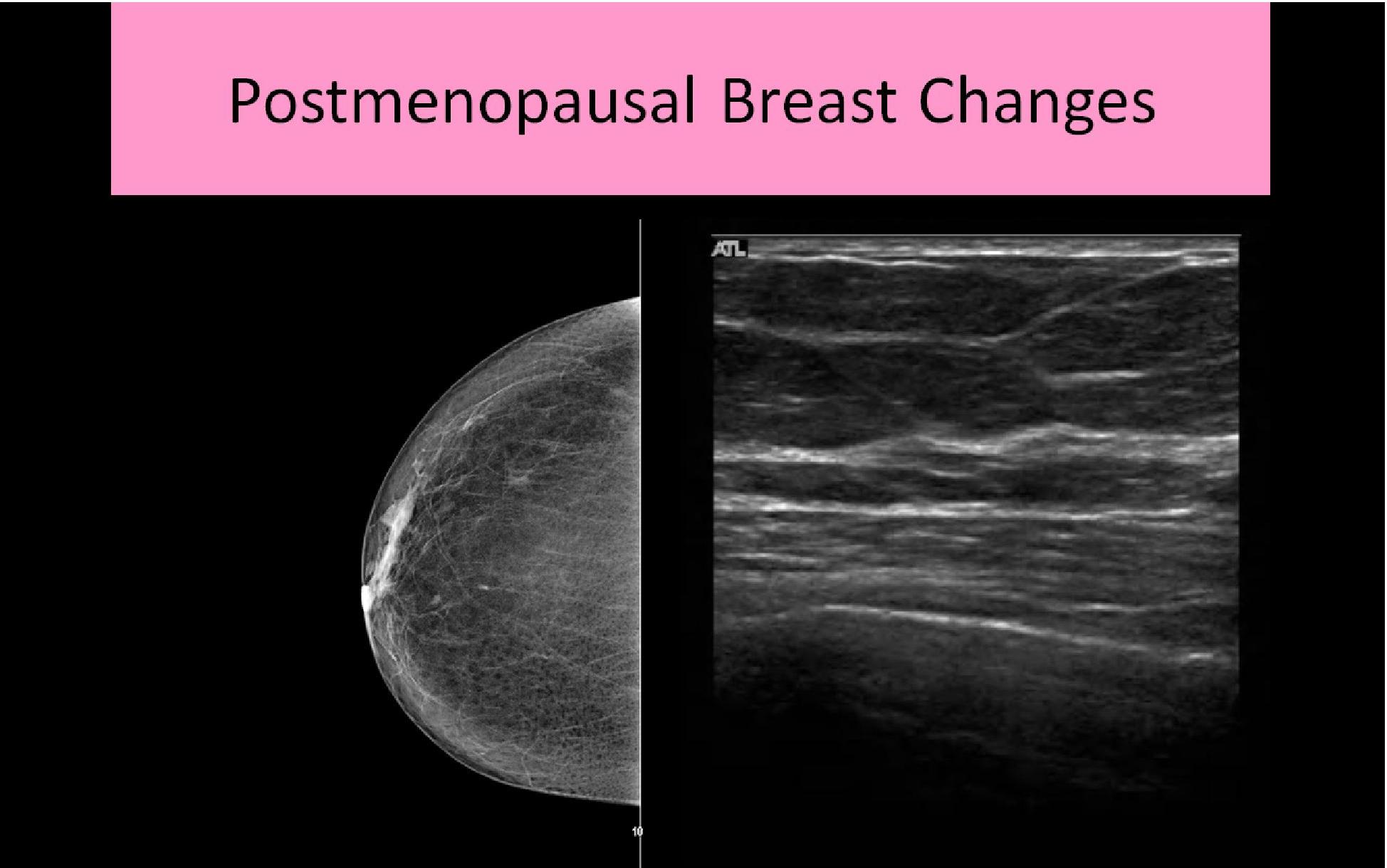
- Postmenopausal: HRT can cause glandular tissue levels to increase; weight loss can lead to prominence of glandular tissue due to the decrease in the amount of surrounding fatty tissue